Is the NHS working on thin ice this winter?
14 February 2019

The NHS in England appears to be having a more manageable winter so far, if the absence of crisis headlines in the media over the last couple of months are to be believed.
However, a close look at the data suggests that it is too soon to draw that conclusion. I’ve looked at three key performance indicators (A&E waits, elective waits and bed occupancy) to explore the change in demand for patient care in hospitals across England over the past few winters.
Positive preparations…
Preparations for winter 2018/19 were broadly similar to last year’s plans. The main priorities were improving take up and effectiveness of the flu vaccine, redirecting patients away from major A&E departments and improving hospital discharge to maximise bed capacity.
The government provided £145m for winter-proofing emergency care in September, 2 months earlier than last year’s funding, which had been criticised as coming too late. However, this year’s money is substantially less than last year’s and it was still received later than trusts would have liked.
…but targets still being missed
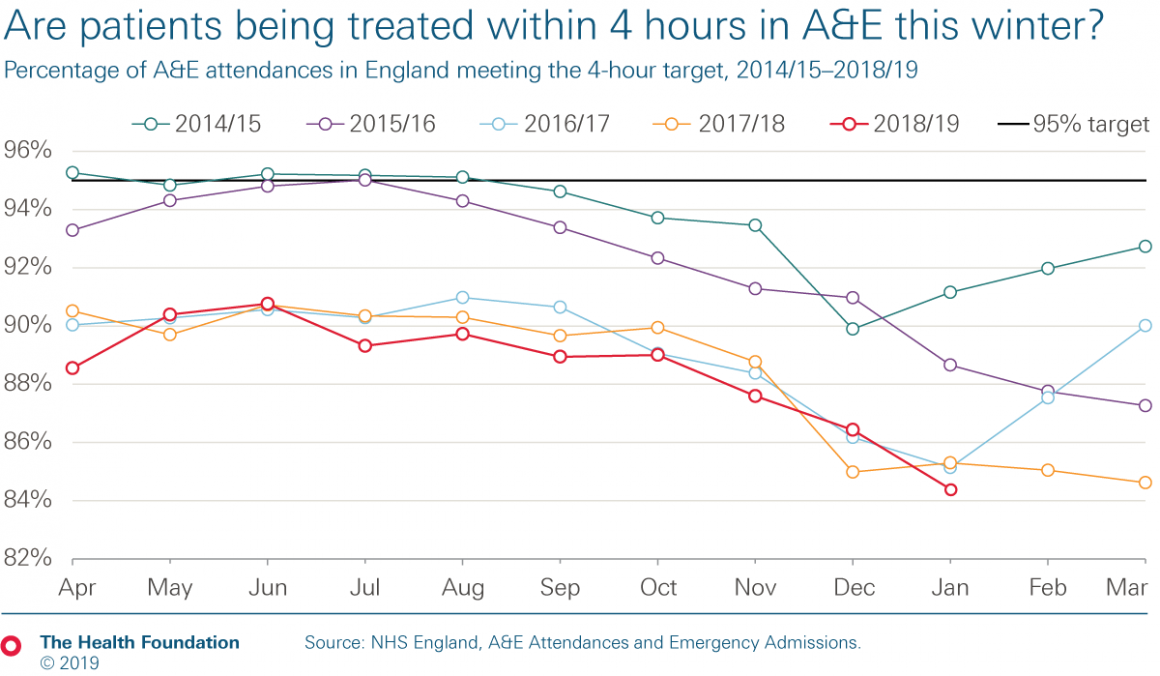
The last 12 months’ data paints a picture of an increasingly busy NHS, where key targets are consistently being missed. Hospitals are expected to admit, discharge or transfer at least 95% of patients within 4 hours of arriving at A&E, but as the chart below shows, this target hasn’t been met consistently at national level in the last 5 years.
While NHS performance in summer 2018 was worse than in recent years, this winter it didn’t drop below the performance of the previous two winters until this January, based on the data released today. However, A&E performance against the 4-hour target is now at its worst ever, at 84.4%.
Consistent with the trends of recent years, last summer saw higher attendance numbers than the winter months of 2018. But this winter, A&E attendance numbers are on par with those of the summer months and are the highest ever seen in January. Growing demand continues to play a part in the rising A&E waiting times, with an average of 71,000 more A&E attendances each month in 2018 than in 2017.
Increased emergency admissions
During every month in 2018, a higher percentage of attendances to major A&E departments led to emergency admissions than in the same month in 2017. For example, in December 2018, 31.2% of patients attending major A&E departments were admitted, whereas 30.1% such cases were admitted in December 2017.
This would suggest that people arriving at A&E are generally more unwell and more need inpatient care than previously, supporting the findings of the Health Foundation’s Emergency hospital admissions in England briefing. This could be (at least partly) the result of more people living with multiple conditions which have greater health care needs (as explained in another recent publication).
Impact of winter pressures on patients
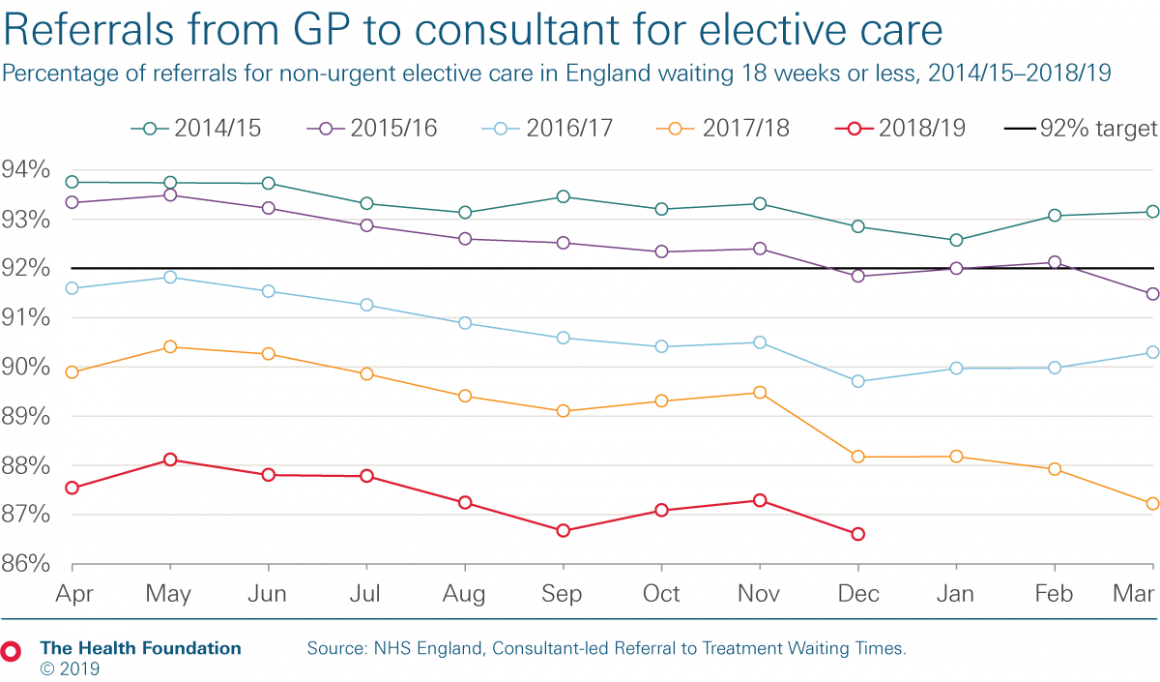
NHS winter pressures inevitably focus on A&E, but we should not forget how winter hits planned treatment too. During last winter, NHS England’s National Escalation Pressures Panel recommended that trusts defer non-urgent elective treatment, but this has not been advised so far this winter. The target is that 92% of patients waiting for such treatment should wait less than 18 weeks after referral from a GP. However, the chart below shows that there has been a steady fall in performance against this target for several years, and so far winter 2018/19 has been no different.
With the elective care backlog being cleared too slowly to improve performance, and the waiting list having grown to an estimated 4.3 million people, this downward trend is set to continue. Elective care may be less urgent, but we must remember how these longer waits for treatment can affect patients, bringing stress and anxiety to their uncertainty and pain (and therefore potentially leading to a lower quality of life, at least in the short term).
The majority of patients admitted for either emergency or non-urgent care will require a general or acute ward bed. Hospital data refers to two types of bed, ‘core’ beds and ‘escalation’ beds. Core beds refer to the hospital’s usual bed stock whereas escalation beds are ones opened by hospitals to create extra capacity in response to high demand. In general, more core beds have been open each week so far this winter, compared to last. But with fewer escalation beds open each week, January 2019 saw fewer total beds available than in January 2018.
Bed occupancy levels affect patient flow through hospitals, and safety can be compromised when bed occupancy levels rise above a certain level. There is debate about what constitutes a ‘safe’ bed occupancy level – whether it is 85% or 92% – but this debate is somewhat academic when current bed occupancy is well over both these suggested limits, with the January average being 94.5%.
The good news and the bad news
Overall, the good news revealed by the data is that the NHS is treating more people than last year, and has so far avoided the crisis headlines seen in previous years. However, the bad news is that performance has continued to deteriorate against a number of important targets. It is possible that we have seen fewer crisis headlines because expectations for emergency performance throughout the winter are now so low. But does slightly better performance in some areas truly equate to good NHS performance?
Some good luck has helped the NHS cope so far this winter, with flu being relatively mild. However, with consistently high bed occupancy and performance still poor, there is little slack in the system, so intense pressure could build up in a short period of time. As today’s data shows, the NHS really is working on thin ice this winter.
Catherine Turton (@CatTurton) is a Senior Analyst in the Quality team at the Health Foundation
Further reading
Work with us
We look for talented and passionate individuals as everyone at the Health Foundation has an important role to play.
View current vacanciesThe Q community
Q is an initiative connecting people with improvement expertise across the UK.
Find out more