Top-down clarity, bottom-up agency: fading freedoms or here to stay?
29 September 2020
Winter is looming. Each year, the winter months bring an uncertain level of additional pressure on NHS and care services. But one thing arrives without fail: intensified central oversight of services (especially emergency services and hospitals), with weekly data published and poor performance amplified in the media. Indeed in some years, there has been extensive top-down planning and management grip on services, from primary care through to emergency departments and hospital discharge services.
The coming months will certainly be more pressured than usual, with the need to manage the backlog of routine care alongside the pandemic that is far from over. But many frontline staff are going into the winter shaped by a very different experience from ‘business as usual’. For sure, the early months of the pandemic brought unforeseen levels of stress, but it was also a time in which many staff were able to rapidly collaborate and come up with new or radically altered services. Leaders at the centre (and the top of organisations), will need to manage the pressures of winter in a way that doesn’t stifle this spirit of ingenuity and autonomy.
Understanding what frees up staff to make change
A rebalancing of relations between the centre and the front line emerged as one of the important enablers for service changes in interviews that informed our recent report: Understanding and sustaining the health care service shifts accelerated by COVID-19.
The report looked at what factors had allowed the rapid adoption of service changes that have long been policy priorities, for example moving away from face-to-face appointments in both primary care and outpatient care.
Many of those interviewed for the report spoke about a shift in relations with the centre, summed up as ‘top-down clarity and bottom-up agency.’ The guidance produced from NHS England and NHS Improvement has been voluminous, extending to primary care, community services and a wide range of hospital specialities, but was characterised as giving a clear idea of the ‘what’ while allowing local organisations to decide on the ‘how’.
Learning from the rapid implementation of video consultations
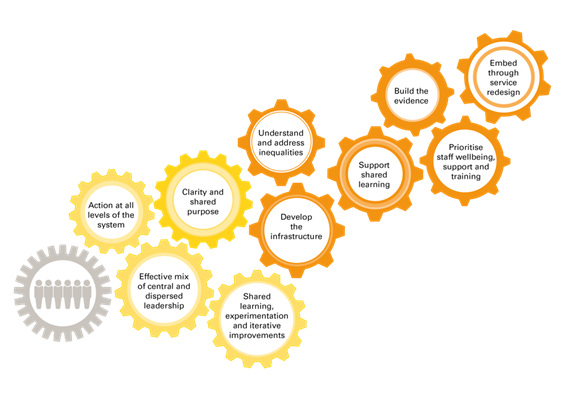
Similar themes emerged from insights gathered through the Q community, from 50 people implementing video consultations. This work showed that leaders need to pay attention to 10 interlinked factors to sustain the momentum behind key service shifts like this.
These are shown in the infographic above, with the yellow cogs showing the four factors that combined to enable the rapid change seen to date.
Clarity and shared purpose were key: the infection risks of face-to-face consultations gave a huge push for staff and patients to switch to video consultations. Action was taken at all levels in the system. Central guidance on governance and centrally commissioned platforms were coupled with a sense of autonomy to make decisions locally. In the absence of clear evidence, and forced to learn as they went, frontline teams found they could make great progress by experimenting and adapting, using improvement methods like PDSA cycles to make informed decisions fast. And people had the space to learn from peers in a way that’s often neglected as a core part of successful change.
As summarised in the six orange cogs, much remains to be resolved for video consultations to become a permanent, high-quality option for the delivery of services. More needs to be known about how they add value to consultations and how to make them accessible to all patients who might benefit from them.
Q found that there is the need to do more to address digital exclusion, supply robust technical infrastructure, and fully understand implications for professional roles.
Taking this learning forward
The challenge now is to transition from the immediate, adrenalin-powered response to the pandemic, to meeting both the challenges of winter and the longer-term need to redesign services. Organisations can only do this by further nurturing the sense of ‘can-do’ frontline agency that emerged during the pandemic.
While this work of improvement is local, sustainable service change requires a parallel process of change to update and align organisational, governance, financial and other processes. During the pandemic, there were big shifts in regional and national systems which were reported to have enabled rapid change, including shifts in regulatory behaviour: suspending CQC inspections, rapidly developed guidance for clinical and information governance that supported greater local freedoms, and a temporary halt to payment by results and other performance management.
At a national level, some of the enabling factors clearly can’t be retained (pandemic pressure or blank funding cheques), but others are worth retaining and developing as NHS and other services consider how to best ‘reset’ post-pandemic.
At our recent webinar we heard concerns that pre-pandemic approaches to payment systems, regulation and governance might re-emerge and ‘solidify’ in a way that once more inhibits innovation and collaboration. Interviewees for our report spoke of the temporary and productive liberation from ‘box ticking’ being slowly eroded by the ‘return of the forms.’
Really understanding and preserving these enabling factors may be challenging at a time when every part of the NHS and wider care system remains under intense pressure as winter approaches, managing COVID-19 and grappling with the backlog of care. But the prize would be worthwhile if the ingenuity and energy of NHS staff shown during the early stage of the pandemic can be harnessed to tackle the many challenges ahead.
Ruth Thorlby (@RThorlby) is Assistant Director of Policy at the Health Foundation and Penny Pereira (@PennyPereira1) is Deputy Director of Improvement at the Health Foundation and Programme Director of the Q initiative.
This content originally featured in our email newsletter, which explores perspectives and expert opinion on a different health or health care topic each month.
Also in this newsletter
Work with us
We look for talented and passionate individuals as everyone at the Health Foundation has an important role to play.
View current vacanciesThe Q community
Q is an initiative connecting people with improvement expertise across the UK.
Find out more