How has hospital use among those clinically extremely vulnerable to COVID-19 been impacted by the pandemic?
24 March 2021
Key points
- During the first wave of the coronavirus (COVID-19) pandemic in the UK, over 2 million people were advised to shield, by staying at home at all times. This group of people have a range of conditions that made them clinically extremely vulnerable (CEV) to serious illness from COVID-19. The CEV population has since been prioritised for vaccines.
- CEV people have complex health needs which require ongoing support from the health and care system. Due to the rapid changes implemented across the system, there is a risk that this group of people experienced particular challenges in access to health and care services. This novel analysis from the Networked Data Lab uses secondary care data linked to the shielded patient list to explore the impact of the first wave of the pandemic on hospital care use by this group of people.
- By examining secondary care use of the CEV population across our five partners, we have highlighted the increasing secondary care use prior to the pandemic and the rapid reduction in use during the shielding period. As the pandemic reached the UK and the shielding programme was implemented, secondary care use dropped rapidly for the CEV population. Comparing April 2020 with April 2019, outpatient attendances fell by between 36% and 47% and elective admissions fell by between 43% and 65% across different regions. For unplanned hospital use, A&E admissions reduced by between 17% and 44% across regions.
- Admissions data indicate that during March to July 2020, between 1.4% and 5.5% of hospital admissions for those considered CEV were linked to COVID-19. However, we know that COVID-19 admissions as captured in the data are likely an underestimate of the true number, due to the slow roll-out of COVID-19 testing and new coding procedures.
- Given that those identified as CEV to serious illness from COVID-19 are a population with complex clinical needs, the substantial fall in secondary care use seen during March to July 2020 is particularly concerning. Missed and postponed care may have resulted in a deterioration in health for this group of individuals. This is particularly important as shielding advice lifts from 1 April in England and Wales, services begin to restart and decisions are made on which patient groups and which services to prioritise.
Introduction
In March 2020, as the COVID-19 pandemic reached the UK, the NHS issued measures to limit certain forms of health care and a national lockdown was announced. As a result of these different measures, hospital use for the general population dropped substantially from March 2020.
During this time, more than 2 million people across the UK were advised to shield by staying at home at all times, as they were identified as clinically extremely vulnerable (CEV) to COVID-19 and at particularly high risk of severe illness. This is a cohort of people with specific and serious health care needs. Missed or delayed care for this population could have significant negative implications for the health of these individuals.
From 1 April, shielding advice is set to lift and the government has stated that formal shielding will only be reintroduced in the worst affected areas for limited periods of time. As services restart and decisions are made on which patient groups and which services to prioritise, the experiences and health service use of this population is an important consideration.
Insights from the Networked Data Lab
The Networked Data Lab (NDL) is a collaborative network of analytical teams across the UK, using linked data sets to help tackle the most important health and care priorities, as identified by both those working in the health and care system and engagement with the public. We use a federated approach to analytics which allows us to conduct analyses on data sets held by different NDL partners and to combine these insights without requiring data to be shared and held in a central location. We work closely with our five partners (Grampian, Leeds, Liverpool and Wirral, North West London and Wales) who are embedded within their local health and care systems and have detailed knowledge of both their local health and care environments and their linked data sets. By working in this way, we are able to conduct rapid and novel analyses that cannot be done at a national level because of a lack of available linked data.
This analysis is the latest in a series from the NDL exploring the impact of the pandemic on the CEV population. Using a federated analytics approach across our five partners, we have analysed secondary care data linked to the shielded patient list to explore the secondary care use of the CEV population between 1 March 2018 and 31 July 2020. This is the first time, to our knowledge, that this issue has been explored across admissions, outpatient and Accident and Emergency (A&E) attendances and was enabled through this novel data linkage and innovative approach. Details on our approach can be found in our statistical analysis plan; and further details on method, inclusion criteria, and data linkage availability, as well as our code, can be found in our GitHub repository. Data on outpatient attendances and A&E admissions were not available for Wales.
Patterns of secondary care use among the clinically extremely vulnerable
There is increasing use of secondary care over 2018 and 2019 among the CEV population, in many cases reaching a peak in January 2020. This likely reflects the evolving complex health needs of this cohort. However, as a result of the pandemic, as well as the policies implemented to deal with the pandemic, the use of secondary care among the CEV population dropped substantially.
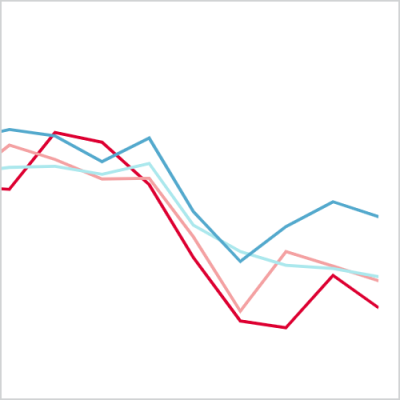
Figure 1
By April 2020, outpatient attendances had fallen by between 36% and 47% across the four partners with data available, as compared to April 2019. Elective admissions fell by between 43% and 65% over the same period. When averaged across partners, this translates to a decrease in outpatient attendances of 43% and a decrease in elective admissions by 51%.
The decrease in unplanned care, while not as large as the decrease in planned care, is still substantial. There was also more variation in patterns of unplanned care use. There were between 17% and 44% fewer A&E attendances in April 2020 compared with April 2019; a 42% decrease when averaged across partners. Across Leeds, Liverpool and Wirral, NW London and Wales, emergency admissions fell by between 26% and 38% (34% averaged across those partners). However, data from Grampian show that the number of emergency admissions in April 2020 was 10% higher than that seen in April 2019, reflecting the steeper rise in the number of emergency admissions among the CEV cohort prior to the pandemic in this area. Nevertheless, the impacts of the pandemic were still evident with the number of emergency admissions falling by 28% between January and April 2020, a pattern similar to other partners.
While there is evidence from NHS Digital that the CEV population experienced a larger decrease in emergency admissions compared with an age-matched general population sample, there is no analysis on how the decreases experienced by the CEV population across other types of secondary care use compared with the general population. To help address this gap, the NDL Grampian team plan to compare hospital use among the CEV population to that of the general Grampian population, as well as considering the impacts of the pandemic on different speciality areas of hospital use. This analysis will be published over the next few months as part of the portfolio of in-depth analysis from NDL partners on the CEV population.
How does the impact of the pandemic differ among the clinically extremely vulnerable?
In our previous analysis, we noted that the age distribution of those identified as CEV was similar between the five NDL partners; around 4 in 10 people were older people (older than the age of 70). Patterns of secondary care use by age prior to the pandemic do not show strong or consistent age-linked patterns across all partners, although outpatient attendance tends to be higher among older people.
The impact of the pandemic on planned care was greater for CEV people who were older. The greatest percentage decreases in activity were for older people: in April 2020, as compared with April 2019, outpatient attendances for this group decreased by between 43% and 53% (49% when averaged across partners) and elective admissions decreased by between 50% and 74% (58% averaged across partners).
Figure 2
In contrast, the largest percentage decrease in unplanned care was for CEV people who are younger than 30 years old: in April 2020 A&E attendances had fallen by between 21% and 66% as compared with April 2019 (62% when averaged across partners). The percentage change in emergency hospital admissions for those younger than 30 who are CEV ranged between a 5% increase (in Grampian, and as explained above) to a 64% decrease in Liverpool and Wirral; when averaged across partners there was a 58% decrease.
Figure 3
This variation in secondary care use by age over the first wave of the pandemic may be due to differences in health care needs; in particular, medical reasons for shielding may vary by age among the CEV population. Evidence from the Strategy Unit shows that in England, reductions in planned care differed by specialty (reductions were more marked in surgical rather than medical specialities); similar patterns are seen in Wales. Differences in the ability to access rapidly reorganised hospital care pathways and the perceived risk of seeking treatment during the pandemic may also play a role in explaining these variations. Understanding whether the observed differences by age are driven by age-linked variation in health care needs or age-linked differences in accessing care requires further, age-stratified analysis into the specific types of planned and unplanned care received by CEV people during this period.
We also found consistent differences in secondary care use by level of deprivation across all five partners, in line with the inverse care law. The proportion of CEV people using planned care (outpatient and elective admissions) is lower among people living in more deprived areas compared to less deprived areas. The reverse is true for unplanned care (A&E and emergency admissions); the proportion of people accessing these forms of secondary care is higher among those living in more deprived areas compared to less deprived areas. These patterns may reflect differences in clinical need, as captured by the variation in medical reasons for shielding by deprivation that we have previously shown, but differences in access to services are also likely to play a role.
Although we do find evidence of the inverse care law in terms of differences in secondary care use, the percentage decrease in secondary care use between March and July 2020 was similar across all levels of deprivation. This suggests that the pre-existing variation in secondary care use persists, but there is no evidence that those living in more deprived areas were disproportionately affected during the shielding period. Given existing evidence on the relationship between deprivation, health and health care use, more detailed analytical models are needed to consider the impact of deprivation while taking account of heterogeneity in medical reasons for shielding, the type of secondary care sought and other demographic factors.
To develop understanding of broader factors which may impact health and health care service use, the NDL Leeds team are undertaking further analysis examining the possible interactions between demographic factors influencing the use of emergency health care for the CEV population and are also exploring how contact with adult social care services has an impact on this group of people. This analysis will be published over the next few months as part of the portfolio of in-depth analysis from NDL partners on the CEV population.
Admissions to hospital for COVID-19
Data on admitted patient care from all partners indicates that, between March and July 2020, 3,920 CEV people had a hospital admission where COVID-19 was recorded. This amounts to 3.9% of CEV people with any hospital admission during this period (range of 1.4% and 5.5% across partners - if a patient was admitted more than once and in different months, they would be counted multiple times in these statistics). The number of COVID-19 admissions will be affected by a number of factors including the exposure risks for each individual to potential COVID-19 infection, for example through an individual’s environment at home; the local COVID-19 case rate, which varied across the UK; differences in how the virus was detected and recorded within local areas; as well as differences in admission thresholds.
It is important to note that this is likely an underestimate of the number of CEV people who had COVID-19-related hospital admissions. During the early stages of the pandemic, testing was heavily restricted due to the limited availability of tests which meant that many cases were likely undetected. New ICD-10 codes for suspected or confirmed COVID-19 were established and rapidly implemented but the use of these codes to record COVID-19 admissions within electronic health records will have taken time to establish. Both of these factors mean that data quality is likely to be varied, making it challenging to effectively identify all COVID-19 admissions within electronic health records during the first few months of the pandemic.
Despite these challenges, understanding COVID-19 admissions among the CEV group is an important element of understanding the experience of this group of individuals through the pandemic.
Deaths of CEV people during the first period of shielding
A total of 8,624 CEV people who were on the shielded patient list across our five partners died during the shielding period of March to July 2020. This is 2.2% of the pooled cohort. It is beyond the scope of this work to consider the reasons for these deaths. The NAO has highlighted the need for further work on mortality as part of evaluating the suitability of the shielding programme, with NHS Digital showing that all-cause mortality for CEV people peaked earlier in the pandemic compared to an age-matched control sample of the general population.
Understanding the implications of changes to hospital use
By examining secondary care use of the CEV population across our five partners, we have highlighted the increasing secondary care use prior to the pandemic and the rapid reduction in use during the shielding period.
The NHS needed to rapidly reconfigure care pathways during the first months of the pandemic, both to ensure sufficient resources to manage the needs of the anticipated influx of patients with COVID-19 and to maintain safety, minimising possible risks of infection to non-COVID patients as well as to staff. The fall in secondary care observed here among the CEV population will be influenced by the evaluation of both clinical need and the importance of minimising the possible risks of infection for each patient. But as this planned care was postponed or cancelled, it is important to assess the long-term health implications of this interruption to care for this population with complex health needs and to interrogate any barriers to access that can be addressed. The experiences of this population during the pandemic of accessing and using health care services is an important consideration in decisions around which patient groups and which services to prioritise as regular NHS services restart.
To build a full picture of the health experiences of the CEV population, these changes in secondary care use should be considered alongside patterns of use in other health care services, including primary and community health care services. It is also important to consider the impact of any unmet health needs on the mental health and wellbeing of the CEV population, particularly in the context of also being asked to shield during this period. The impact of the shielding programme on mental health has been an important issue for many, and three of the NDL partners (Liverpool and Wirral, North West London and Wales) are planning further analyses to understand more about the mental health and mental health care access for the CEV population. These analyses will be published over the next few months as part of the portfolio of in-depth analysis from NDL partners on the CEV population.
This long chart was co-authored by the team members of the five NDL partners, led by Alisha Davies (Wales), Jessica E Butler (Grampian), Sara Sekelj (NW London), Simon Chambers (Liverpool and Wirral) and Frank Wood (Leeds). Each partner contributed to the development of the statistical analysis plan for this work, curated and analysed the data from their own area and reviewed this description of the work. Further detail can be found on GitHub. This work uses data provided by patients and collected by the NHS as part of their care and support.
Further reading
Work with us
We look for talented and passionate individuals as everyone at the Health Foundation has an important role to play.
View current vacanciesThe Q community
Q is an initiative connecting people with improvement expertise across the UK.
Find out more

