How are changes to employment and finances impacting mental health during lockdown?
25 June 2020
Key points
- This analysis explores how changes in people’s economic circumstances relate to their mental health during the early lockdown period. It uses data collected in a YouGov survey of 6,005 respondents between 6 and 11 May.
- In the early lockdown period survey results show that, overall, people of working age (18–65) were more concerned about their own or their family’s mental health (62%) and physical health (65%) than they were before the outbreak began. And people were more concerned about these than their household finances (48%).
- People experiencing a worsening in their family’s finances during lockdown were more likely to be highly or very highly concerned with their family’s mental and physical health than when finances had stayed the same or improved.
- 46% of respondents were found to have poor mental health. This was more common among young people (aged 18–24), women, single people and renters. While these patterns pre-date the current crisis, other research suggests greater deterioration in mental health for young people and women relative to other groups since lockdown.
- Regardless of income, the likelihood of poor mental health was higher if families had experienced a deterioration of their finances during lockdown or expected one in the next 3 months. However, in the poorest 20% of families almost three-quarters (72%) reporting a worse financial position had poor mental health, compared to around half (48%) in the richest 20%.
- People who were still working or had been furloughed were less likely to report poor mental health than those who had lost their jobs since lockdown. Retaining a job through being furloughed may have helped prevent a rise in unemployment-related mental health problems. Given the negative health consequences of unemployment, the government should be ready to extend the furlough scheme as necessary to prevent a sharp rise in unemployment. This could better protect household incomes and ultimately our nation’s health.
Introduction
The unprecedented measures taken to control the spread of coronavirus (COVID-19) have had major economic, social and health impacts, with those already disadvantaged often being the hardest hit. While many of the impacts on health will become more apparent over the coming years, there are also short-term impacts that need to be considered now. In particular, the lockdown period – which began in the UK on 23 March – has led to a general worsening of mental health and reduced wellbeing. People have reported higher levels of anxiety and lower levels of happiness and life satisfaction.
This analysis explores how changes in people’s economic circumstances have impacted on their mental health during the early lockdown period using data collected between 6 and 11 May 2020. This analysis draws on a survey designed and commissioned by the Resolution Foundation, in partnership with the Health Foundation (although the views in this analysis are not necessarily those of the Resolution Foundation). It was conducted using an online interview administered to members of the YouGov Plc UK panel, made up of over 800,000 individuals who have agreed to take part. The total sample size was 6,005 adults, aged 18–65. Figures relating to the proportion of those experiencing poor mental health, wellbeing measures, changes in employment status and income distribution have been analysed independently of YouGov by the Health Foundation and are not the views of YouGov. Analysis of the income distribution follows the method developed by Resolution Foundation.
Rates of poor mental health increased during the early part of lockdown
Our analysis of the YouGov survey suggests a significantly higher proportion of working age adults (aged 18–65) have experienced poor mental health (46%) during lockdown compared to surveys using comparable methods conducted in previous years (around 20%).
The measure of mental health is created from the General Health Questionnaire-12 (GHQ-12) – a validated and widely used measure of common mental health symptoms in population studies (see Box 1 for further details). An increase in the reported level of people experiencing poor mental health has been found in other research using the same measure of mental health, although the share of the population reporting them in our analysis is higher (see Box 1). Given the snapshot nature of the YouGov survey, we focus on how mental health and wellbeing differs between groups and varies by economic situation during lockdown.
Data collected since early May suggests some improvement in mental health and wellbeing, potentially as people have adjusted to lockdown measures and following the easing of some rules, though levels remain elevated above usually-reported outcomes. However, it is important to understand potential drivers of poor mental health during the response to COVID-19 and the groups in most need of support.
The YouGov survey uses the GHQ-12 set of questions – a suite of 12 questions used to identify poor mental health. Questions focus on areas such as the ability to concentrate, whether people feel they are playing a useful role and whether they feel under strain. Responses to each question are scored and then combined to create a measure of mental health. In our analysis of the four possible responses to each question, the two indicating worse mental health are scored as a ‘1’, the others a ‘0’. A threshold of four from across all 12 questions is used to indicate if an individual had experienced poor mental health.
We compared the YouGov survey data used in this analysis to the UKHLS (Understanding Society) April 2020 wave, also collected during lockdown but at the end of April. Comparing the two sets of results, the YouGov survey reported a higher proportion of people indicating poor mental health, but both surveys displayed similar patterns by age and sex. The variation between groups was slightly greater using UKHLS.
These differences in the overall level of reported mental health problems between surveys should be taken into account when interpreting the findings. However, the focus of this analysis is on the relative differences between groups, rather than the absolute level of poor mental health.
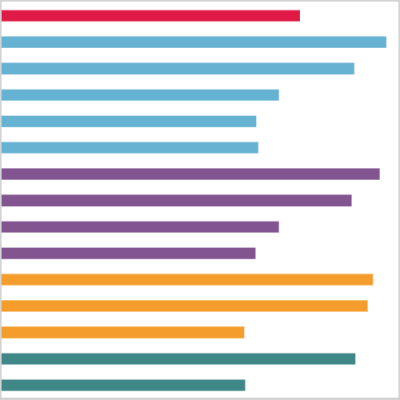
Women and younger people are more likely to have suffered poor mental health
Figure 1 shows the proportion of different groups with poor mental health in early May. People younger than age 35 and women were particularly likely to have poor mental health, which to an extent reflects pre-lockdown differences in the prevalence of poor mental health found in other surveys. However, research using UKHLS suggests that the rise in mental health issues has been relatively greater among women and younger age groups since the COVID-19 pandemic.
Single people (where the relationship status is single, but may be living with a parent or in a multi-adult household) and non-homeowners also had a relatively higher share showing poor mental health. To some extent this may be expected given requirements to distance from others and not socialise with other households.
Renting is also associated with worse mental health, stemming from the stress that can be caused by the insecurity of the private rental sector. Younger people are also more likely to privately rent and be single creating a potential avenue through which the mental health effects of COVID-19 measures are compounded. Higher housing costs for private renters create pressure on incomes, however support from government for renters has been limited during lockdown. This may have heightened stress and anxiety for those suffering a fall in income since lockdown in a way that homeowners, who could access mortgage payment holidays, would not have experienced.
Any such exacerbation of existing differences in mental health, and the underlying drivers of those differences, are important to understand so that support can be put in place to prevent a widening of health inequalities in the event of further instances of lockdown and beyond the current crisis.
Employment, furloughing and job loss
Perhaps the most obvious economic shock to individuals during the pandemic has been changes to employment, with many experiencing a loss of pay or hours or the loss of a job altogether. We would expect that such changes to income or work status might cause a deterioration in mental health. Our analysis shows that losing a job is associated with poorer mental health but this is not the case for furloughing.
Figure 2 shows the GHQ-12 indicator of mental health and standard questions about wellbeing – How satisfied are you with your life nowadays? How happy did you feel yesterday? How anxious did you feel yesterday? – against change in employment status since lockdown.
People who have been furloughed, and therefore retain a continued attachment to a job and potentially less of a shock to their income, report similar levels of mental health and happiness as people who have continued to work. There were significantly greater differences in poor mental health and happiness between people no longer working due to job loss, and those still working or furloughed. There was a significant difference in the share reporting low life satisfaction between people who had lost a job and those still in work, but not between people with either of those groups and those being furloughed.
Concern over family health and finances
In the early lockdown period, overall, people of working age (18–65) were more concerned about their own or their family’s mental health (62%) and physical health (65%) than they were before the outbreak began, and are more concerned about these than their household finances (48%).
Figure 3 shows that the extent of people’s concern for their family’s physical or mental health and wellbeing corresponds to a change in their financial situation. While there was generally high concern about health across the population, concern was greater the more a family’s finances were reported to have worsened – and regardless of their income level.
Over two-fifths of people reporting deteriorated finances had ‘very high’ concern over their family’s physical or mental health. If a family’s finances had ‘worsened a lot’, the respondent was almost half as likely again (45%) to report high concern with their family’s mental health than where their finances had improved a lot.
Low income and financial uncertainty
The prevalence of poor mental health was patterned by incomes. People living in low income families and experiencing a worsening of their financial position had a higher likelihood of reporting poor mental health.
Analysis in this section utilises the method developed and set out by the Resolution Foundation in Return to spender. It is based on the income position of 18–65-year-old adults, excluding any families containing retired adults or non-working adult students immediately prior to the COVID-19 outbreak. We compare mental health outcomes across quintiles of equivalised family income.
As Figure 4 shows, a higher share of people living in the poorest fifth of families had poor mental health (55%) than in the richest fifth (38%). In families where their financial position was felt to have worsened, the proportion of people with poor mental health was higher across the income distribution. However, 72% of people living in the poorest fifth of families who reported a deterioration in their finances, experienced poor mental health compared to 48% of those living in the richest fifth of families reported a deterioration in their finances.
These findings should also be considered in the context of the substantial support for incomes provided by government since the outbreak. The standard allowance in Universal Credit was increased by £20 a week, while the Job Retention Scheme has helped protect incomes by providing 80% of earnings (up to a cap of £2,500 a month) for furloughed workers (the majority of which live in middle-income families). Without such support a larger number of families would likely have experienced a worsening or greater worsening in their financial position.
Conclusion
There is abundant evidence that loss of income, spending time in poverty and unemployment have a negative impact on health. Recognition of the need to tackle a rising prevalence of mental health problems has been growing in recent years. In the midst of a pandemic, and one of the greatest and most sudden economic shocks the UK has experienced, it is important to ensure the impact on the nation’s mental health is taken into account in decision making.
Studies related to the impact of COVID-19 have found that the lockdown period has led to higher rates of poor mental health. This has partly been related to the measures put in place limiting normal social interaction, but is also linked to the economic consequences of those measures. The substantial support provided by the Coronavirus Job Retention Scheme to protect the incomes of workers, may have helped prevent a job loss-driven mental health crisis.
As the government considers measures to stimulate economic recovery, it will be important to ensure that sufficient support for workers is available. That is why the government should be ready to extend the furlough scheme if necessary. This could prevent an otherwise potential sharp rise in unemployment leading to a likely worsening in mental health. The measures taken to protect incomes and restore the economy will be key in determining the future health of the country.
David Finch (@davidfinchrf) is a Senior Fellow at the Health Foundation.
Alexandra Eastaugh is an Analyst Intern in the Healthy Lives team at the Health Foundation.
Further reading
Work with us
We look for talented and passionate individuals as everyone at the Health Foundation has an important role to play.
View current vacanciesThe Q community
Q is an initiative connecting people with improvement expertise across the UK.
Find out more

