How has COVID-19 affected service delivery in GP practices that offered remote consultations before the pandemic?
16 July 2020
- Care provision in GP practices has dramatically changed due to COVID-19. Remote consultation has been rapidly introduced to protect patients and staff from the risks of infection.
- askmyGP is an NHS-approved remote consultation supplier. We look at 51 GP practices using askmyGP prior to March 2020, and explore how primary care access, supply and demand has varied during COVID-19. These early insights reveal some of the potential advantages of and challenges to effective remote consultation.
- Consultation rates at askmyGP practices decreased by less than 1% between 1 March–30 June 2020, compared to the same period in 2019. Month on month changes for March, April, May and June in 2020 compared to 2019 were +3%, 0%, -15% and +11% respectively. Pre- and post- lockdown in March, consultation rates decreased by up to 17%, from 3.77 to 3.14 per person per year.
- In contrast, national data suggests falls of up to 6%, 33% and 33% in March, April and May (latest available) respectively compared to 2019 figures, and up to 30% during March 2020.
- At askmyGP practices, there has been a dramatic swing away from face-to-face consultations. Between 1 March–30 June 2020, 8.5% of appointments were held face-to-face, compared to 38% during the same period in 2019. Conversely, use of remote consultation methods increased. Telephone appointments increased from 39% to 51%, online message from 23% to 40% and although video increased 50-fold, it remained low at 0.5%.
- Between 1 March–30 June 2020, patients at askmyGP practice aged under 4, 5–15, and 15–24 years had 11%, 21% and 10% fewer appointments respectively, compared to the same period in 2019. During the same timeframe there were 9% more consultations for askmyGP patients aged 75+ years.
- Our results suggest practices familiar with conducting appointments remotely were able to adapt quickly to the demands of COVID-19 and undertake more care remotely without significantly impacting the total number of consultations delivered. As the pandemic has progressed, these practices have demonstrated resilience by responding flexibly to variations in demand for care throughout April to June.
- These results point to the benefits of using digital technology in general practice and suggest the NHS should continue to invest in digital-first primary care. Doing so in the short term may make primary care more resilient to future waves of the virus. However, research is required to answer questions about the impact of remote consultation on the quality of care, patient experience and access, and workload.
- We also need to understand under which circumstances patients can benefit from video consultations. The Health Foundation is commissioning further research to inform the longer-term sustainability of video consultations and the Q Community has published insights into tackling its impact on health inequalities.
Because of COVID-19 most GP practices have had to dramatically change how they provide care for their patients. Under NHS guidance, remote consultation (via telephone, online message or video) has been rapidly introduced to replace face-to-face consultation.
The data presented in this analysis is based on practices where remote consultation had already been introduced before the outbreak of the COVID-19 pandemic. At these practices, patients were able to use online tools to access primary care services in line with the strategy set out in the NHS Long Term Plan. Looking at the demand for care in these practices and how they were able to adapt to provide flexible access to services during COVID-19 provides early insights into the potential advantages of and challenges to remote consultation, and may help to guide future NHS policy in the event of a second wave of the virus.
Background
The NHS Long Term Plan set out an ambition to offer digital-first primary care – where patients use online tools to access primary care services remotely – to most people by 2023/24. The latest GP contract requires that all patients have the right to online consultation by April 2020, and video consultation by 2021. However, there has been reluctance to implement remote consultations because of concerns about their potential impact, particularly on patients’ privacy and safety, healthcare inequalities and GPs’ workloads.
The Royal College of GPs (RCGP) reported that, before the lockdown on 23 March 2020, approximately a quarter of GP appointments were carried out remotely. COVID-19 changed that. Practices were required to reduce avoidable footfall, and to protect patients and staff from risk of infection. This necessitated major and immediate changes to how general practice works. On 5 March NHS England issued the first in a series of regular updates to general practice regarding the pandemic with advice to change face-to-face appointments booked online to triage appointments via telephone or video. On 19 March, further guidance was issued urging practices and commissioners to move to a total triage system (wherein every patient is triaged before making an appointment) and to provide as much care as possible remotely. A complete timeline of national policy and health system responses to COVID-19 in England is available in our policy tracker.
Some practices were ahead of the game
The NHS has approved 34 suppliers of remote triage and online consultation. One of these is askmyGP, provided by GP Access Ltd. askmyGP offers a complete workflow system which manages all incoming patient contacts. Patients contact their practice via a link from the practice website. They can: request a consultation, stating a preference for consultation type via face-to-face, telephone, online message or video; and upload clinically relevant information (such as a photograph). Non-digital users are taken through the same process by practice staff over the phone. Clinicians and staff then prioritise and deliver care according to patient preference and needs.
Before the COVID-19 pandemic, 51 practices were using askmyGP for all patient contacts. As part of a wider evaluation of digital-first primary care, the Improvement Analytics Unit, a partnership between NHS England and Improvement and the Health Foundation, has access to summary data records of 1.8 million GP appointments between 1 March 2019–6 July 2020, from practices using askmyGP. In examining this data, it is important to note that each record corresponds to an opening consultation request and only captures the final consultation type – it therefore may not include all interim interactions between the GP and patient. Further, these practices are not representative of the whole country, as they have an average list size larger than the national average, a larger-than-average number of full-time-equivalent GPs and are located in predominantly urban areas skewed towards serving patients in the least-deprived quintiles. However, the data is useful to estimate consultation rates and to look at how primary care access, supply and demand has changed before and after the outbreak of COVID-19.
Consultation rates before COVID-19
Between 1 March–30 June 2019, these established askmyGP practices delivered the equivalent of 3.26 consultations per person per year. Patients aged 75+ years had the highest consultation rate (4.92 per person per year) and those aged 5–14 years had the lowest (1.52 per person per year). These rates are lower than national reports – for example, a study of 100 million consultations in England estimated a GP and nurse consultation rate of 5.16 per person per year for 2013/14 – but mirror trends reported in that study across ages and gender.
37% of these askmyGP consultations were delivered face-to-face, 1% by home visit (based on July–October 2019 data), 39% by telephone, 23% by online message and 0.01% by video. In summary, these practices were already delivering 62% of consultations remotely before the pandemic, compared to approximately 25% nationally (as estimated by the RCGP). These data suggest that askmyGP practices were already aligned with NHS strategy on remote consultations, and likely to be in a good position to adapt and respond quickly to the new COVID-19 guidance.
How have patients been using primary care services at askmyGP practices during the COVID-19 pandemic?
The overall consultation rate dipped in early March but averaged about the same as 2019 during the pandemic
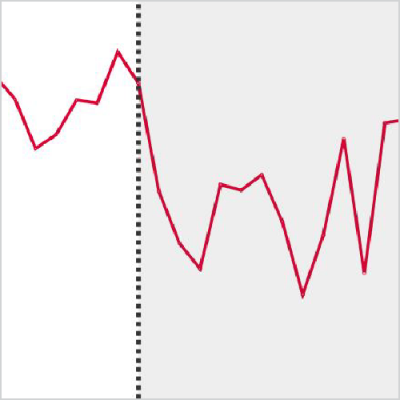
Between 1 March–30 June 2020, the average consultation rate per person per year in askmyGP practices was 3.25. This is a decrease of less than 1% from the same period in 2019, when the average rate was 3.26. Month on month changes for March, April, May and June in 2020 compared to 2019 are +3%, 0%, -15% and +11% respectively. Pre- and post- lockdown on 23 March 2020, consultation rates decreased by up to 17%, from 3.77 (week commencing 2 March 2020) to 3.14 (week commencing 30 March 2020) per person per year.
These decreases are smaller than that suggested nationally, where reports indicate falls of up to 6%, 33% and 33% in March, April and May 2020 respectively compared to the same period in 2019, and by up to 30% between the first and last weeks of March 2020. Although these national data may not count other kinds of appointments taking place, such as in hubs, or telephone triage, they may reflect a drop in the number of patients contacting their GP.
Rates continued to decrease during April over Easter (weeks commencing 6 and 13) but recovered slightly in the week commencing 20 April 2020. By the week commencing 18 May, rates had decreased to a pandemic low of 2.43 per person per year, after which they climbed erratically towards the end of May and throughout June. An NHS campaign launched on 25 April, which encouraged patients to seek the medical care they needed, might be the cause of recovery during this month. The trends from the end of May and throughout June may signal varying levels of confidence as the first and second steps in easing the lockdown were taken on 13 May and 1 June respectively.
Fewer face-to-face appointments
In line with COVID-19 guidance, there was a dramatic swing away from face-to-face consultations. At askmyGP practices between 1 March–30 June 2020 only 8.5% of appointments were held face-to-face – either in the surgery (8%) or at home (0.5%) – in comparison to 38% during the same period in 2019. In April, just 2.6% of appointments were conducted face-to-face, compared to 36.8% the year before – a swing of 34%.
Conversely, remote consultation methods increased. Telephone appointments increased from a constant 39% in March, April, May and June 2019 to 43%, 55%, 55% and 53% in March, April, May and June 2020 respectively. Online messaging increased from an average of 23% between 1 March-30 June 2019 to 40% between 1 March-30 June 2020. Video increased 50-fold over the same period, however it remained low at 0.5%. Notably, the proportion of appointments where an attachment was uploaded increased from 3% in March 2020 to 8% in June 2020. Given the restriction on face-to-face consultations, this may indicate a preference for discussing a photograph by online message or telephone call rather than a video consultation.
Fewer appointments for younger patients, more appointments for older patients
Between 1 March–30 June 2020 there were fewer consultations for younger patients at askmyGP practices compared to the same period in 2019. Children aged under 4 years and 5–15 years, and young adults aged 15–24 years had 11%, 21% and 10% fewer appointments respectively. The decrease was particularly evident during May 2020 where rates for these groups dropped by 29%, 38% and 24% respectively in comparison to May 2019.
In general, these lower rates may be related to a reluctance to access care for fear of catching the virus or feeling like a burden on the NHS, or due to widespread advice that coronavirus is rarely serious in children. Further, a survey of 2,000 children and young people aged under 25 years found that in some cases younger patients were anxious about talking on the phone or via video.
In contrast, during the same timeframe there were 9% more consultations for patients aged 75+ years. This increased rate may reflect the fact that older patients, who are more likely to have underlying conditions, are more concerned by advice that they are at increased risk and that clinicians, encouraged by Age UK, are proactively reaching out to these groups.
What do these data tell us?
Our analysis reveals early evidence to suggest that practices familiar with conducting appointments remotely were able to adapt quickly to the demands of COVID-19. They were able to undertake more care remotely without significantly impacting the total number of consultations. As the pandemic has progressed, these practices have demonstrated resilience by responding flexibly to variations in demand for care throughout April–June, pointing to a benefit of using digital technology in general practice and suggesting that the NHS should continue to invest in digital-first primary care. Doing so in the short term may make primary care more resilient to future waves of the virus.
Patient groups responded differently during the early months of the pandemic. Younger patients had fewer appointments, and, regardless of the reasons, may not have had all the care they needed; older patients had more appointments and may have benefitted from the use of remote consultations for management of long-term conditions. More studies are required to answer questions about the impact of remote consultation on quality of care, patient experience and access. Understanding the implications for practice workload will also be critical.
As argued in the Health Foundation’s report The spread challenge, successful innovation in one place is unlikely to be replicated elsewhere if simply rolled out without accounting for the local context. The Health Foundation has outlined three key quality considerations for remote consultations and the Improvement Analytics Unit is performing a wider evaluation of the impact of different models of digital-first primary care.
Finally, although the concept of video as a tool for consultation is gaining headway, it only increased marginally in use during the pandemic at askmyGP practices whereas the proportion of appointments where an attachment was uploaded more than doubled. More research is required to understand under what circumstances photographs are an adequate substitute for video consultation. The Health Foundation is commissioning further research to inform the longer-term, post-COVID-19 spread and sustainability of video consultations and the Q Community has published insights into tackling its impact on health inequalities.
The Health Foundation will be publishing further analysis exploring primary care usage during the COVID-19 pandemic in the coming months.
Acknowledgements
We thank askmyGP for sharing their data for this analysis.
Further reading
Work with us
We look for talented and passionate individuals as everyone at the Health Foundation has an important role to play.
View current vacanciesThe Q community
Q is an initiative connecting people with improvement expertise across the UK.
Find out more

