The continuing impact of COVID-19 on health and inequalities
A year on from our COVID-19 impact inquiry
The continuing impact of COVID-19 on health and inequalities
Key points
- A year on from publication of the Health Foundation’s impact inquiry, inequalities in COVID-19 mortality persist with mortality rates 3 to 4 times higher in the most deprived areas. However, the overall number of COVID-19 deaths is now significantly lower than it was during the first year of the pandemic.
- The vaccination programme has been key to reducing COVID-19 mortality rates, but for some groups uptake is still low, especially for people living in poorer areas and people from some minority ethnic groups.
- The significant deterioration in mental health during the first year of the pandemic has been reversing but has not entirely returned to pre-pandemic levels. Data suggest that anxiety remains heightened, especially among women. People are likely to be less resilient to cope with the stress associated with financial strain in the growing cost-of-living crisis.
- A large rise in unemployment was avoided, largely due to government support through the furlough scheme. However, long-term health conditions are keeping a significant number of people out of work, representing an ongoing challenge for government and the economy, as well as for individuals.
- There has been a failure to act on education gaps due to lost learning time in the pandemic. These are between children from richer and poorer backgrounds and compared with previous cohorts. A cohort of ‘left-behind’ children face significant risks to their long-term health and living standards, as well as causing a long-term economic cost to the country.
Introduction
In July 2021 we published our COVID-19 impact inquiry, providing an initial assessment of how the pandemic affected health and health inequalities during its first year. The report found that poor health and existing inequalities had left parts of the UK more vulnerable to the virus and had influenced its devastating impact. It also found that the pandemic has highlighted stark differences in the health of the working age population – with those younger than 65 in the poorest 10% of areas in England almost four times more likely to die from COVID-19 than those in the richest. The inquiry report concluded that the recovery needs to prioritise creating opportunities for good health – a vital asset needed to 'level up' and support the economy.
At the time of writing the report in May 2021, around a quarter of the population had experienced at least one COVID-19 infection, and just over half of UK adults had been vaccinated twice. We highlighted the effect of the pandemic on health and inequalities, but also explored how policy helped to mitigate some of these, while pointing to future risks to health.
A year on, 90% more than 90% of the UK population have had at least one COVID-19 infection, and 74% of adults had received three vaccinations by April 2022. The terms of reference for the statutory public inquiry have now been set. This inquiry will play a crucial role in understanding how the UK can prevent another human, social and economic disaster on the scale of that caused by COVID-19. The size and complexity of the task cannot be underestimated.
Here, we revisit the conclusions of our COVID-19 impact inquiry to consider the further direct impact of COVID-19 on health outcomes and the broader implications for health and the wider determinants. We also discuss the extent to which previously highlighted risks to health have been addressed and the implications for the country of ‘living with COVID-19’.
Direct effects on health
COVID-19 mortality
COVID-19 remains a significant cause of death in the UK in this latest phase of the pandemic: in the first 6 months of 2022, 13,500 people died due to COVID-19 (4.9% of all deaths) and 20,300 people’s deaths where COVID-19 was mentioned on the death certificate but may not be the main cause (7.3% of all deaths). This is considerably lower than in 2020 and 2021, when the population had lower levels of immunity through vaccination and to a lesser extent infection. For comparison, a typical flu year in the UK has averaged around 28,000 deaths since 2000.
For most of the pandemic, excess mortality has been a better measure of the impact of COVID-19, due to the absence of community testing in early 2020. Excess mortality indicates how many people have died relative to expectations, typically by comparing to historical averages. Figure 1 shows how the UK (highlighted red) has fared compared to other OECD countries in excess deaths per 100,000 people since March 2020.
As of June 2022, the UK had experienced a cumulative 204 excess deaths per 100,000. In March 2022, when there are comparable data for most countries, the UK ranked 15th out of 33 available OECD countries for the highest cumulative excess mortality. Among OECD countries, the UK fared poorly by the end of 2020, ranking 4th out of 33 for excess deaths in this period. A delayed lockdown in winter 2020 contributed to a significant rise in excess deaths. There has been considerable improvement since then, due to the vaccine rollout and relatively high uptake, with the UK ranking 11th out of 33 countries with available data in the OECD in June 2022 in vaccinations administered per person.
One of the consequences of the pandemic has been a sharp fall in period life expectancy in 2020. However, it is important to note that this does not mean that COVID-19 will lead to significantly shortened life spans in future. Period life expectancy is calculated based on current age-specific mortality rates applying over the lifetime. Assuming that the higher mortality rates of 2020 and 2021 are temporary, then period life expectancy can also be expected to return to pre-COVID-19 levels. The future challenge then becomes how to reverse the pre-pandemic trend of stalled improvements in life expectancy.
Inequalities in COVID-19 mortality by deprivation
The absolute number of COVID-19 deaths has reduced, but there is still a significant gap in the risk of dying from COVID-19 between people from the most and least deprived areas. Since July 2021, both age-standardised mortality rates and the absolute number of COVID-19 deaths have been consistently higher in the most deprived areas (Figure 2).
Age-standardised COVID-19 mortality rates have generally been around three or four times higher (in a given month) in the most deprived areas than in the least deprived. Between July and December 2021 there were 2,300 COVID-19 deaths in the most deprived areas of England, 2.5 times more than the 900 in the least deprived areas.
Inequalities have also remained among people from different ethnic backgrounds, although the latest data are only available up to February 2022. In the Omicron variant wave, Bangladeshi and Pakistani men and women have had mortality rates between two and three times higher than white British men and women, while mortality rates for black Caribbean men and women of mixed ethnicity are also higher than for white British men and women respectively.
Our impact inquiry showed the key factors associated with these patterns of deaths, including increased risk of exposure to the virus and pre-existing poor health. Risk of exposure may no longer be a key factor at this stage in the pandemic: the FT estimated that in April around 90% of the UK population had been infected with COVID-19, and the MRC Biostatistics Unit estimates there have been around 67 million COVID-19 infections as of July 2022, with the vast majority (around 52 million) occurring in the past 12 months. However, underlying health remains a key factor. People aged 50–69 years living in the 10% most-deprived areas are twice as likely to have two or more long-term conditions than those in the 10% least-deprived areas.
The vaccination programme
The reduction in COVID-19 mortality rates and excess mortality has in large part been driven by the vaccination programme, which has offered between three and five jabs to all UK adults and two jabs to 5–15-year-olds. As Figure 3 shows, the UK initially had a very speedy rollout of vaccines in 2021 although this is now equivalent to or slightly below other western European countries with around 220 COVID-19 vaccinations per 100 of population.
Despite the high overall level of vaccination there are inequalities in coverage, particularly when it comes to booster jabs. Figure 4 compares the age-standardised vaccination rate between different groups. The three or more vaccination rate is 20 percentage points higher in the least deprived areas than in the most deprived areas (81% to 61%). Those whose first language is not English are also less likely to have been vaccinated or have received a booster. People from most minority ethnic groups are less likely than white British groups to have received three shots, with around 40% of African Caribbean adults not having received any COVID-19 vaccination accounting for age. The UKHSA monitoring reports show the continued effectiveness of COVID-19 vaccination against hospitalisation and mortality, particularly for boosters.
COVID-19 illness
Long COVID
Long COVID refers to persistent symptoms lasting months after initial infection. One study drawing on the experiences of people with long COVID found a list of over 200 symptoms, but the most common symptoms were fatigue brought on by physical or mental activity, memory and cognitive problems.
Measuring how many people experience long COVID is difficult. The best-known data source in the UK is the ONS survey on self-reported long COVID. The survey tracks the number of people self-reporting 12 common long COVID symptoms continuously over a period of at least 4 to 12 weeks, which gives an estimate of around 2% of people in the UK experiencing long COVID at least 12 weeks after infection in July 2022. The ONS has also investigated methods such as experiencing any COVID-19 symptom at least 12 weeks after infection and self-reported long COVID, which provided prevalence estimates of 5% and 12% in September 2021. In the case of any one symptom, 3.5% of the control group who had not had COVID-19 also reported having these symptoms, indicating they can be common in the population generally. Other studies that include control groups tend to find lower incidences of long COVID.
While the ONS survey may be an overestimate of long COVID prevalence, it does reveal interesting trends and inequalities. The first is that the vaccination programme appears to have reduced the risk of a given infection leading to long COVID – something that appears in academic studies (eg Ayoubkhani et al 2022) – but also clear from observational data. In March 2021, the ONS survey suggested around 930,000 people in England had long COVID. By June 2022, this number was 1.6 million. Based on the MRC Biostatistics estimates, by March 2021 there had been 13 million COVID-19 infections, and 62 million COVID-19 infections by June 2022. Comparing the two very approximately suggests the first 13 million infections led to 930,000 cases (around 1 in 14), while the next 49 million infections led to around 700,000 instances of long COVID (around 1 in 70). This is not to downplay the severity of long COVID when it arises, with a large proportion reporting severe limitations on day-to-day activities. Nearly three-quarters (72%) of people on the ONS measure of long COVID report limitation in their day-to-day activities, posing a large health burden.
The incidence of long COVID on this measure is also unequal. Figure 5 shows that self-reported long COVID incidence is higher for those in more deprived areas, people of white ethnicity, those aged 35–69 years, and in particular, those whose pre-existing health was limited by conditions. Those with pre-existing health conditions have also seen the largest absolute increase in long COVID prevalence between March 2021 and June 2022.
Indirect effects on health
Health care
Throughout the pandemic the NHS has been under huge pressure. The need to refocus provision towards severe cases of COVID-19 and the wider restrictions in place meant that by July 2021 there were 7.5 million fewer people referred into consultant-led elective care. The pressure has continued with only 73% of people attending A&E departments in December 2021 and February 2022 seen within 4 hours, compared to a target of 95%. Only 63% of patients waiting for an elective (planned) treatment in February were within 18 weeks of a referral compared to a target of 92%. By June 2022 the waiting list for routine hospital care had reached 6.5 million, with 323,000 patients waiting over a year.
There are a number of reasons for these continued pressures. Their persistence is not purely due to the additional demand created by the pandemic – such as the wave of COVID-19 hospitalisations through winter 2021–22. Bed capacity has also been more limited due to infection prevention control measures and staff absence rates increased with the wave of COVID-19 infections in late 2021.
However, some of the disruption relates to the changes to care that has been required in dealing with COVID-19 compared with the NHS’s traditional low length of stay, high occupancy model. Other pressures, including a backlog in primary care and difficulty discharging patients into social care settings, have added to disruption. Workforce shortages represented the single biggest challenge facing the NHS in England well before COVID-19. But the pandemic has driven increased demand for health care, growing waiting lists and a substantial elective care backlog, while impacting negatively on staff wellbeing and absence.
Mental health
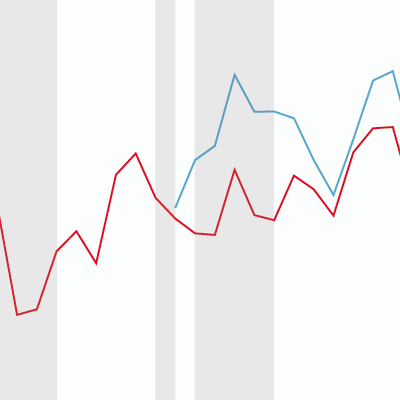
With huge changes to day-to-day life in the UK during the pandemic, there were significant reductions in mental health. This is reflected in ONS measures of wellbeing, which were first collected in 2011. As Figure 6 shows these significantly worsened at the start of the pandemic. By the third quarter of 2021 these had moved back towards 2019 levels although levels of self-reported anxiety remained higher than before the start of the pandemic driven by higher anxiety among women.
A recent study by Natcen concluded that although overall levels of worry in Britain were at similar levels in 2022 to the pre-pandemic position, a gap has opened up between men and women. Women are now more likely to be worried about aspects of their lives than before the pandemic. Other studies highlighted links between worsening mental health and concerns over finances or employment and actual deteriorations in these factors. Parental mental health has also been shown to have an impact on children’s mental health in adulthood. The experience of the pandemic may have reduced resilience to further crises, with some people less able to cope. This places greater urgency on concerns about consequences of the cost-of-living crisis for mental health.
Risk factors
The impact of the first 2 years of the pandemic on risk factors for ill health – such as alcohol and tobacco – is still not fully known. But where information is available early signs are that some may have worsened and inequalities widened. For instance, drug and alcohol-related deaths rose in 2020, and physical activity levels reduced, particularly for people from more disadvantaged backgrounds. The latest obesity statistics for children show an unprecedented increase in obesity rates – 25.5% of 11-year-olds were obese in 2020/21, an increase of 4.5 percentage points on 2019/20. Inequalities remain wider with prevalence of severely obese children in the most deprived areas increasing by more than in the least deprived areas.
At the same time the public health system – already stretched by the pandemic – was reorganised, leading to the formation of the Office for Health Improvement and Disparities (OHID), as well as the health protection focused UK Health Security Agency (UKHSA). This meant further disruption at a time of national public health crisis. Meanwhile investment in the public health grant, cut by almost a quarter on a per person basis since 2015/16, has still not been prioritised. As with other public services, higher than expected inflation at the time spending plans for 2022/23 were committed to will mean a real-terms cut this year.
Wider determinants: three key risks for future health
The greatest influence on our health are the wider determinants of health. These are the conditions in which we are born, grow, live and work. Here we focus on three key areas affected by the pandemic that we identified as potential risks to future health in the COVID-19 impact inquiry.
Education and lost learning
By the end of the 2020–21 spring term primary school children had lost between 2 and 2.3 months of reading progress and between 3.1 and 3.6 months of progress in maths. Secondary school pupils experienced similar levels of learning loss for reading, amounting to 1.6 and 2 months respectively for years 8 and 9.
A recent evidence review by the Education Endowment Foundation suggests that the attainment gap between disadvantaged students and their peers has grown. And while there has been some recovery in learning since summer 2021, pupils overall are not performing as well in maths and reading as pre-pandemic cohorts.
Limited further data are available, although recent Department for Education statistics indicate attainment by the end of key stage 2 (10–11-year-olds). On all areas tested, apart from reading, children are performing at lower levels than their pre-pandemic counterparts.
The IFS has estimated a potential lifetime loss in earnings of £350bn in relation to missed education, but relative to the potential long-term consequences government policy in this area has been limited. Initial funding to help children ‘catch up’ was described as inadequate. A total of nearly £5bn has now been announced to help children through a mix of catch-up premiums and tuition programmes in England. This compares with annual day-to-day spending on schools of around £50bn in England.
It will take time to know whether children have been able to catch up on learning. One guide to progress is the rollout of catch-up support. The education select committee found significant regional variation in the success of delivering additional tuition. By March 2021 the National Tutoring Programme had reached 100% of its target numbers of schools in the South West of England and 96.1% in the South East. But it had reached just 58.8% in the North East, 58.9% in Yorkshire and the Humber, and 59.3% in the North West. National Tutoring Programme official statistics show that overall 80% of schools in England had accessed some provision under the programme by July 2022, an increase on the March 2022 figure of 60%.
The pandemic has also had a significant impact on pupil attendance. Restrictions limited the time children could spend in school, but even with schools fully open cases have also led to periods of lower attendance and higher staff absence. If further outbreaks of COVID-19 lead to similar school disruption, this could cumulatively amount to a significant loss of learning. Previous research has shown a strong link between pupil absence and lower attainment. New or enhanced approaches will likely be needed to ensure schools can cope with catch-up or continued hybrid learning.
Employment and economic inactivity
At the start of the pandemic, as widespread restrictions were introduced, the risk of high unemployment became a major concern. Businesses closed and social measures prevented some people from being able to work. Significant government support in the form of the Coronavirus Job Retention Scheme (CJRS) or furlough scheme helped to prevent the rise in unemployment many feared, and the unemployment rate is now back to pre-pandemic levels.
However, levels of economic inactivity have worsened. An additional 520,000 people aged 16–64 years were economically inactive in the 3 months to June 2022 compared with the 3 months to February 2020, around two-thirds of the change has been for those aged 50–64.
Figure 8 shows the change in economic inactivity for people aged 50–69 years by reason. Our analysis shows that by Q1 2022 the single largest increase was driven by long-term sickness and disability (100,00 people). The other larger increases were for people looking after home or family (75,000) and those who reported that they do not need employment (65,000). These are the self-reported ‘main reason’ for inactivity. People may prefer not to report a different reason, or be inactive due to a more complex set of factors.
Our initial analysis suggests that changes in the absolute number of people in economic inactivity is mostly driven by an increased in the likelihood of inactivity, but a small component is also an increase in the size of the population aged 50–69 years since 2020. However, in Q1 2022 there were 7 million people with a condition that limited the amount of work they could do, which has grown by 2 million since the late 1990s. Several recent pieces of work have painted a somewhat contradictory picture of whether the increase in inactivity is being driven by early retirement or ill-health, something we plan to unpick in future work. Higher inactivity levels could have significant consequences for growth and the public finances through a limited labour supply and reduced income generation. It will be important to understand the barriers to work for this group and effective policy responses to boost employment.
One factor that remains unclear is the impact of long COVID on labour market outcomes. Analysis by the IFS for 2021 found around 1 in 10 workers with long COVID went on long-term sick leave, with relatively few losing employment. This was equivalent to around 110,000 workers, with the longer term effects unclear but potentially dissipating. Other recent academic estimates based on the Labour Force Survey and the ONS long COVID survey suggest around 96,000 people leaving employment due to long COVID. There is still work needed to understand the longer term employment prospects of people with long COVID.
COVID-19 sickness absence
The ONS estimates that in 2021, 2.2% of working days were lost to sickness absence – the highest rate since 2010. COVID-19 was responsible for around 24% of these sickness days across the year, equivalent to 35.8 million days. This does not necessarily mean that this will be the ‘settled’ COVID sickness absence rate for the next few years.
The presence of ongoing lockdowns and restrictions in the first part of 2021 reduced mixing between people, depressing the potential rate of COVID-19 and other sickness absence. Because the population was less exposed to COVID-19 through infection and vaccination throughout the year, sickness absence could be lower in future due to higher levels of immunity.
Changes to rules around self-isolation will also influence the level of absence, as will the frequency and severity of future variant-driven waves of infection. It will be important that state provision, such as statutory sick pay, and employer practices are adapted to fairly take into account any increased rate of sickness absence in future. Some employers, particularly those in service industries and the delivery arms of the public sector (including the NHS), may also need to adapt staffing approaches – such as having more flexible on-call staff – to cope with temporary labour shortages.
Income and family finances
As with concerns about unemployment, significant government support – largely through the CJRS and the £20 per week uplift to Universal Credit – meant that the potentially large effects of restrictions on income have tended, on average at least, to be mitigated. Analysis by Resolution Foundation found that median incomes for working age families were estimated to grow in real terms by 1.5% in 2020/21, with lower income working age families faring particularly well due to the support put into place in the first year of the pandemic.
However, the experiences of individuals and families have varied. There were rises in some measures of deprivation at the start of the pandemic and many reported financial concerns during the pandemic. In part this reflected a lack of resilience before the pandemic, in the 2 years prior more than 1 in 4 adults said they would not be able to manage for a month if they lost their main source of income. By June 2021, a survey funded by the Health Foundation and designed by Resolution Foundation showed that 16% of working age individuals’ savings had fallen, rising to 32% of people on the lowest incomes and 22% of people in the second-lowest fifth of income.
Having endured 2 years of the pandemic, families’ financial positions are set to be severely tested by the cost-of-living crisis. This will have significant implications for health, including through the risk people are unable to afford essentials such as sufficient heat and food, and through the stress associated with financial strain.
Rising energy prices are driving high inflation, expected to peak at over 13% by the end of 2022. Lower income families will be most exposed given essentials represent a greater share of their spending. In May government set out large-scale support that would broadly offset the average increase in energy bills expected at that time. However, larger families are likely to have higher than average energy costs; cost pressures are growing on other areas of spend, such as food; and latest expectations suggest energy prices will increase by more in October than anticipated when measures were first set out. Further help will be necessary for families to cope.
The precarious position of many lower income families largely reflects historical policy choices to reduce the value of support provided through the social security system, as well as cuts to public service provision. This has also been a factor in determining the scale and shape of the additional support required during the pandemic and in the current cost-of-living crisis.
Conclusion
The COVID-19 pandemic led to an unprecedented shock to all aspects of our lives and has had a significant impact on the current health of the UK. The pandemic has evolved in a way that poses risks to future health as well. It will still be a long time before the full effects are understood given the multiple ways the factors that influence our health have been affected. There is even some way to go to fully grasp the direct impact of COVID-19 on health, particularly in relation to how the virus mutates with time, the long-run efficacy of vaccination and the true extent of long COVID.
Some impacts are already clear. The societal and political reaction to the pandemic has shown the power of policy action to address social ills. Large-scale programmes of vaccination and financial support have broadly been a success. But the disproportionate effects of the pandemic on some groups reflect existing societal fault lines, with the failure to address historical inequalities exacerbating the impact for many. We also know that COVID-19 deaths continue to be more likely in the most deprived areas and that there are clear gaps in vaccination coverage.
Despite this knowledge there is still a significant risk that these unequal effects continue as the country learns to live with COVID-19. Further disruption could have a significant impact on recovery, particularly in tackling the NHS backlog. One major risk to longer term health is education. Evidence to date suggests gaps between children from richer and poorer backgrounds that widened during the pandemic are likely to persist. There has been limited action to bring education levels back in line with pre-pandemic expectations. The inadequacy of the catch-up funding combined with the long-term implications for individuals and society make education an area of significant policy failure.
Changing political leadership presents an opportunity to refresh and refocus efforts. The delayed health disparities white paper remains an important vehicle to make progress and commit to a long-term strategy and action to tackle poor health and health inequalities. The same poor underlying health that increased the vulnerability of the UK to the pandemic in the first place.
Further reading
Share this page:
Work with us
We look for talented and passionate individuals as everyone at the Health Foundation has an important role to play.
View current vacanciesThe Q community
Q is an initiative connecting people with improvement expertise across the UK.
Find out more

