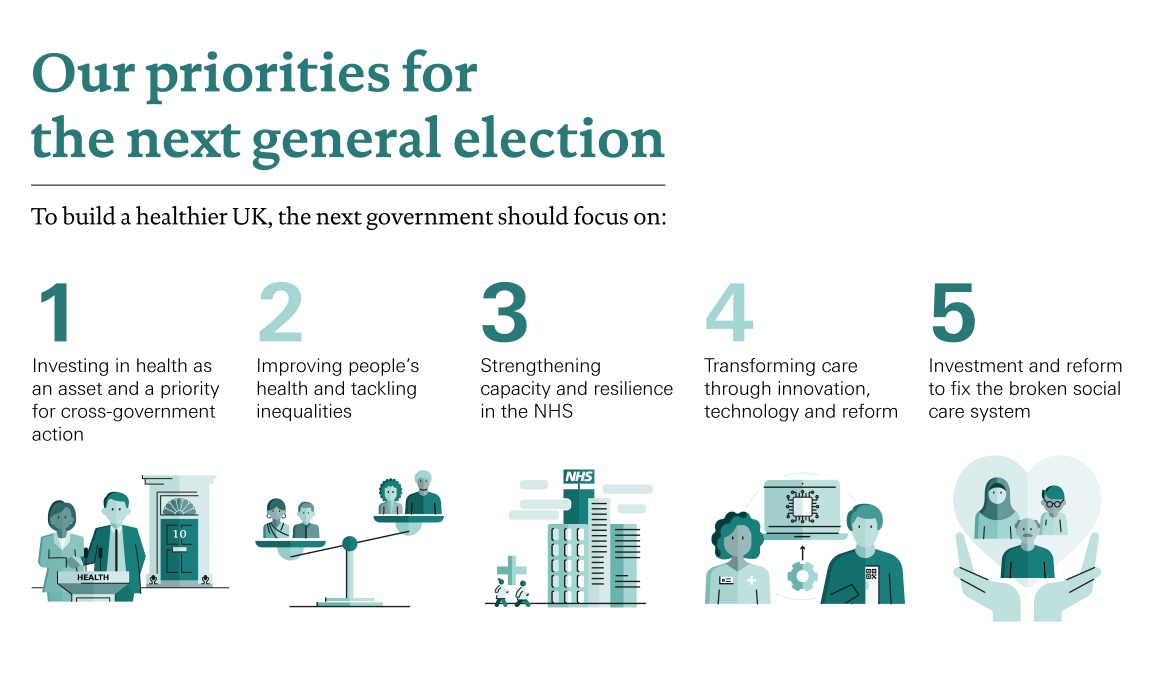
General Election Our views and analysis on health and social care for the 2024/25 General Election

Successive governments have failed to invest in the nation’s health, and neglected wider economic and social factors that form the building blocks of our health. Now the UK’s health is fraying, the NHS is in crisis, and people are struggling to get the care they need. So what must the next government do?
The collection below pulls together our work on the most pressing priorities for health and care, making the case for policy changes to build a healthier UK.
Read more
Health is our most precious asset. Good health and wellbeing enables people to achieve their potential, fuels the economy and helps build a stronger society. Yet, successive governments have failed to invest in the nation’s health and have neglected the wider economic, social and environmental factors that form the building blocks of our health. As a result, our health is fraying, while an ageing population and changing patterns of disease mean that many more people will be living with major illness in future, with profound implications for the NHS, other public services and the public finances.
The NHS was not set up to go it alone. Improving people’s health depends on a wider system of public services and support including local government, housing and social security that were decimated by a decade of austerity, with the NHS often left to pick up the pieces. Insufficient emphasis is placed on prevention, leaving too many people with preventable illness and increasing demand on the NHS. A new approach is needed that values the role good health plays in the prosperity, resilience and fabric of the nation, places it at the heart of national policy decisions and takes a ‘whole-government’ approach to coordinating action.
Priorities for action
- A bold, ambitious goal to improve the nation’s health to sit alongside the net zero target and increasing economic growth as the key drivers of government policy over the next decade and beyond.
- Ensure that improving the nation’s health is baked into government decision-making by introducing new legislation to enshrine this new goal in law and establish a new independent body to monitor and drive progress.
- A cross-government strategy, backed by strong leadership from the Prime Minister, to drive action across Whitehall to address the wider determinants of health.
- A shift to prevention to reduce the impact of illness, support people to live healthier lives and reduce demand for NHS services, backed by changes to Treasury rules to ring-fence spending and ensure prevention is prioritised.
- Ensure that new regional and local bodies, and efforts to promote economic and social development, incorporate a strong focus on reducing health inequalities.
The UK has fallen down the international league table for life expectancy and compares poorly on key outcomes such as cancer and heart disease, while deep inequalities in health between our poorest and wealthiest communities are widening. Trends for some of the major risk factors to people’s health are going in the wrong direction, more people are living longer with major illness and mental ill health has increased significantly. Yet successive governments have shied away from taking the bold action needed to improve the population’s health and tackle inequalities. Record numbers of people are out of the workforce due to ill health, while the number of people in work who report work limiting health conditions has increased significantly. This is shrinking the labour force and holding back economic growth. Local government has a vital role to play in creating healthy places and communities but endured severe cuts during the years of austerity, with public health budgets taking a significant hit. Business also has an important role to play by addressing the commercial determinants of health and promoting healthier workplaces. Experience suggests that it is possible to make significant gains in improving population health and tackling inequalities if bold and coordinated action is taken.
Priorities for action
- Address the big risk factors that shape health outcomes – smoking, alcohol use, diet and physical inactivity – at a population level, including bolder use of tax and regulation, stronger support for local action and a focus on addressing the wider determinants of health.
- A coordinated, systematic approach to tackling health inequalities, learning from evidence of what worked in the past.
- Reduce economic inactivity and improve health for people in work by taking coordinated action to address barriers to work due to ill health, increase support for those out of work as a result of illness and disability, and work with business to support employee health, keep people in work and promote healthier workplaces.
- Increase local government funding and change the way that resources are allocated to ensure that more investment in the NHS and other public services is targeted at the most deprived areas with the worst economic and health outcomes.
- Increase public health budgets to boost investment in vital local public health services.
The NHS is in crisis and many people are unable to get the care they need. Pressures are being felt right across the system, with record waiting lists for hospital treatment, lives being lost due to the strain on urgent and emergency services and people struggling to see their GP. Health systems across the world face significant challenges and have been disrupted by the Covid-19 pandemic but the causes of the NHS crisis pre-date this. Going into the pandemic, a decade of low spending growth and a focus on relieving short-term pressures at the expense of long-term investment, left the health service with chronic staff shortages, insufficient capacity and inadequate buildings, equipment and IT. At the same time, a larger proportion of the NHS budget was spent on hospital care and a declining share on prevention, primary and community care.
In recent years, the NHS has struggled to increase productivity, and activity in hospitals has not risen in line with recent increases in funding and staff, while the average length of stay in hospital has increased and too many beds are occupied by patients who are medically fit to be discharged. Public satisfaction with the NHS is at an all-time low, but the public strongly support its founding principles and there is no case for radical changes to its funding model. There are no quick fixes, but the NHS can recover with a mix of policy change and investment over the long term.
Priorities for action
- Provide stable, long-term investment to meet underlying demand and cost pressures, increase capacity and strengthen the resilience of the NHS.
- A renewed drive to increase productivity in the NHS based on a thorough understanding of the factors that are currently holding it back.
- A once-in-a-generation capital settlement to transform the NHS into a 21st century service and help improve productivity by modernising crumbling buildings, replacing outdated equipment and investing in the new technology and digital infrastructure needed across the NHS, including in primary care.
- Build on the NHS Long Term Workforce Plan through a long-term commitment to funding the expansion of workforce training it sets out, legislating to update projections of future workforce needs and boosting staff retention by taking stronger action on pay, conditions and workplace cultures.
- A new deal for primary care to tackle the mismatch between demand and capacity by increasing the share of NHS investment it receives, recruiting more GPs and other practice staff and tackling the ‘inverse care law’ that leaves practices in poorer areas underfunded and under-doctored compared to richer areas.
Stable, sustained investment in capital and infrastructure, more staff and the adoption of new technologies are critical but, on their own, not enough to deliver the changes needed to transform services and meet future health and care needs. Previous reforms to the NHS have focused too much on top–down structural changes and not enough on changing how care is delivered and experienced. While progress is being made in integrating care, radical innovation and improvement is needed to deliver on longstanding policy objectives to provide more coordinated care for people with multiple conditions, focus on prevention and deliver more care in people’s homes and communities. This should be based on supporting health and care staff to innovate, with a focus on speeding up testing, evaluating and spreading improvements in care. The scale and structure of the NHS as a national single payer health system means it is in a unique position to capitalise on these opportunities. It will also be vital to harness the potential created by advances in AI, data and technology to improve productivity, as well as improve the quality and experience of care, and support the shift to a more preventive and personalised health and care system.
Priorities for action
- A new approach to reform that avoids further top–down structural change and instead focuses on supporting staff to improve care, with clear national priorities and better alignment of policy, including targets and payment systems.
- A bold, nationally coordinated approach to transform the delivery, quality and experience of care through faster development, evaluation, adoption and spread of new innovations across the NHS.
- Build on progress in integrating care by improving the coordination of services for those with multiple health conditions, increasing the focus on prevention and supporting people to manage their own health by providing more care in people’s homes and communities.
- A renewed focus on delivering systematic and continuous improvements in services by giving front-line staff freedom and support to innovate, backed by national action to help spread good practice.
- A new strategy to accelerate the development and adoption of AI across the NHS, alongside effective regulation, support for staff to develop the digital and analytical skills they will need and a focus on digital inclusion for all patients.
The adult social care system in England is failing the people who need it. State-funded care is a threadbare safety-net and only available to people with the highest needs and lowest means, while many face potentially catastrophic costs. Services are under extreme pressure, with high levels of unmet need, patchy quality of care and an unstable provider market. This places a heavy burden on families and friends to plug the gaps in a broken system by providing informal care, often with limited support. Pressures in social care have a knock-on effect on the NHS, contributing to delays in patients leaving hospitals. The sector is facing a workforce crisis – vacancies are high, pay and conditions are poor, and care workers experience high levels of poverty and deprivation. Despite the pressing need for change, successive governments have failed to reform social care, leaving a catalogue of broken promises, delays and abandoned manifesto commitments. Continued inaction would mean choosing to prolong one of the biggest public policy failures of our generation.
Priorities for action
- Fundamental reform of adult social care funding and entitlements in England to provide fairer and more generous state protection against the costs of care, pooling risk across the population.
- Increased investment in the current system to improve access to publicly funded care and tackle unmet need, support providers to improve services and meet growing demand for care.
- A fully funded long-term workforce strategy to expand the social care workforce and improve pay and conditions for staff.
- Expanded access to breaks and other support for unpaid carers to help them balance caring and other responsibilities and improve their health and wellbeing.
Work with us
We look for talented and passionate individuals as everyone at the Health Foundation has an important role to play.
View current vacanciesThe Q community
Q is an initiative connecting people with improvement expertise across the UK.
Find out more