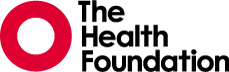
In deprived areas, patients referred for psychological therapy are less likely to receive treatment
- Improving Access to Psychological Therapies (IAPT) is an ambitious programme to deliver psychological therapies at scale within England, which began in 2008. As part of a commitment to address the historical under-investment in mental health services, the NHS Long Term Plan included plans to treat 380,000 more patients per year through the IAPT programme.
- There is variation in who is affected, for example men in the lowest income households are three times more likely to have a common mental disorder than men in the highest income households. But referrals from patients in deprived areas are less likely to receive a course of treatment than those in wealthier areas.
- Building the evidence base of current inequalities is key to ensuring that the push to expand access to mental health care services serves those who most need support.
IAPT is an ambitious programme to deliver psychological therapies at scale within England, which began in 2008. It is often regarded at the best at-scale roll out of these treatments worldwide. By 2018/19, there were 1,495,680 referrals to IAPT and 38.9% of these completed a course of treatment. 52.1% of treated patients recovered, matching recovery rates demonstrated in the controlled environment of clinical trials — an ambitious goal for the service to have achieved.
As part of a commitment to address the historical under-investment in mental health services, the NHS Long Term Plan included plans to treat 380,000 more patients per year through the IAPT programme.
Policies to expand access to treatment should be good news for addressing health inequalities. We examined publically available data to try and understand how the likelihood of receiving treatment following a referral varies by level of deprivation. As the chart shows, currently referrals from patients in deprived areas are less likely to receive a course of treatment than those in wealthier areas.
Given the health inequalities evident in the publicly available data, we want to do further work to build a more granular picture of how waiting times, symptom severity and treatment delivery mode might affect how patients progress through the pathway, and how this varies between different patient groups.
Building the evidence base of current inequalities is key to ensuring that the push to expand access to mental health care services serves those who most need support.
Further reading
Work with us
We look for talented and passionate individuals as everyone at the Health Foundation has an important role to play.
View current vacanciesThe Q community
Q is an initiative connecting people with improvement expertise across the UK.
Find out more