Longer hospital stays and fewer admissions
How NHS hospital care changed in England between 2019 and 2022
Longer hospital stays and fewer admissions
23 June 2023
-
Over the two decades before the pandemic, the number of NHS patients admitted to hospital increased year-on-year, despite a reduction in the number of hospital beds. Since the COVID-19 pandemic, fewer patients have been admitted to NHS hospitals and length of stay has risen, raising questions about NHS productivity, quality of care and the prospects of meeting ambitions to recover services.
-
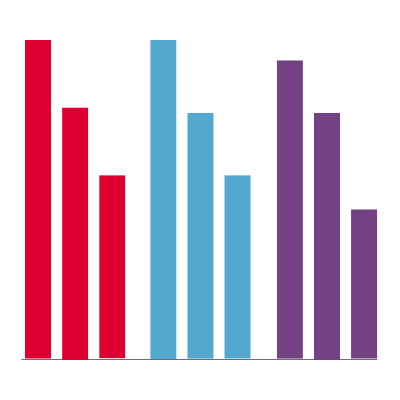
In 2022, there were 800,000 (12%) fewer hospital admissions than in 2019, with elective admissions down by 279,000 (21%) and emergency admissions by 521,000 (9%). Despite this, the number of bed days has declined only slightly by 2.5%, from 36.2 million in 2019 to 35.3 million in 2022.
-
Average length of stay in hospital increased from 7.3 days in 2019 to 8.3 days in 2022 (13%). Length of stay for emergency admissions grew from 7.9 to 9.1 days (15%), while length of stay for elective admissions decreased slightly from 5.2 to 5.1 days (3%).
-
There were 41,000 (8%) more emergency admissions lasting more than 14 days in 2022 than in 2019. With hospitals already operating at or near capacity, this resulted in a reduction in the number of shorter stays, with 560,000 (11%) fewer emergency admissions lasting up to 14 days in 2022 than in 2019.
-
While the number of emergency admissions fell and average length of stay increased for all age groups, the most significant change was among older patients, with average length of stay increasing from 10.8 to 12.5 days among those aged 85 years and older.
-
Although emergency admissions fell in all areas, the most significant reductions were seen among people living in the most deprived areas, who also experienced the greatest decreases in elective admissions. This raises significant concerns about inequalities in access to care and whether commitments made by national leaders to tackle health inequalities are being met.
-
Our analysis indicates, in response to pressures on beds and longer hospital stays, that hospitals have been forced to increase admissions thresholds, in effect rationing care by admitting fewer patients. It is not clear what has happened to more than half a million patients who would have been admitted for short emergency stays in 2019. Some are likely to have been treated elsewhere, potentially increasing the pressure on other services, while some are likely to have gone untreated.
-
This is further evidence of a system operating under intense strain. While we cannot be certain about the combination of factors that explain these trends, it is evident that insufficient hospital capacity and barriers to patient flow – including high bed occupancy, delays in discharging patients and the continued need to treat patients with COVID-19 – have played a significant role. It is clear that reductions in hospital beds went too far.
-
Policymakers have set ambitious targets for recovering NHS service standards that are predicated on hospital services working more productively to treat more patients. Understanding the factors contributing to the fall in hospital admissions and increase in length of stay – and whether they are amenable to intervention – will be critical to achieving these targets.
Further reading
Work with us
We look for talented and passionate individuals as everyone at the Health Foundation has an important role to play.
View current vacanciesThe Q community
Q is an initiative connecting people with improvement expertise across the UK.
Find out more

