Which technologies offer the biggest opportunities to save time in the NHS?
Which technologies offer the biggest opportunities to save time in the NHS?
29 April 2024

Key points
- In the face of huge demand pressures, technology presents a significant opportunity to support workforce capacity in the NHS, as recognised in the 2024 Spring Budget and NHS Long Term Workforce Plan. Drawing on new Health Foundation research – including a UK-wide clinical staff survey and expert interviews – this analysis spotlights clinicians’ views about which technologies might help the NHS boost productivity and release time for care, and sets out what steps will be important to realise these gains.
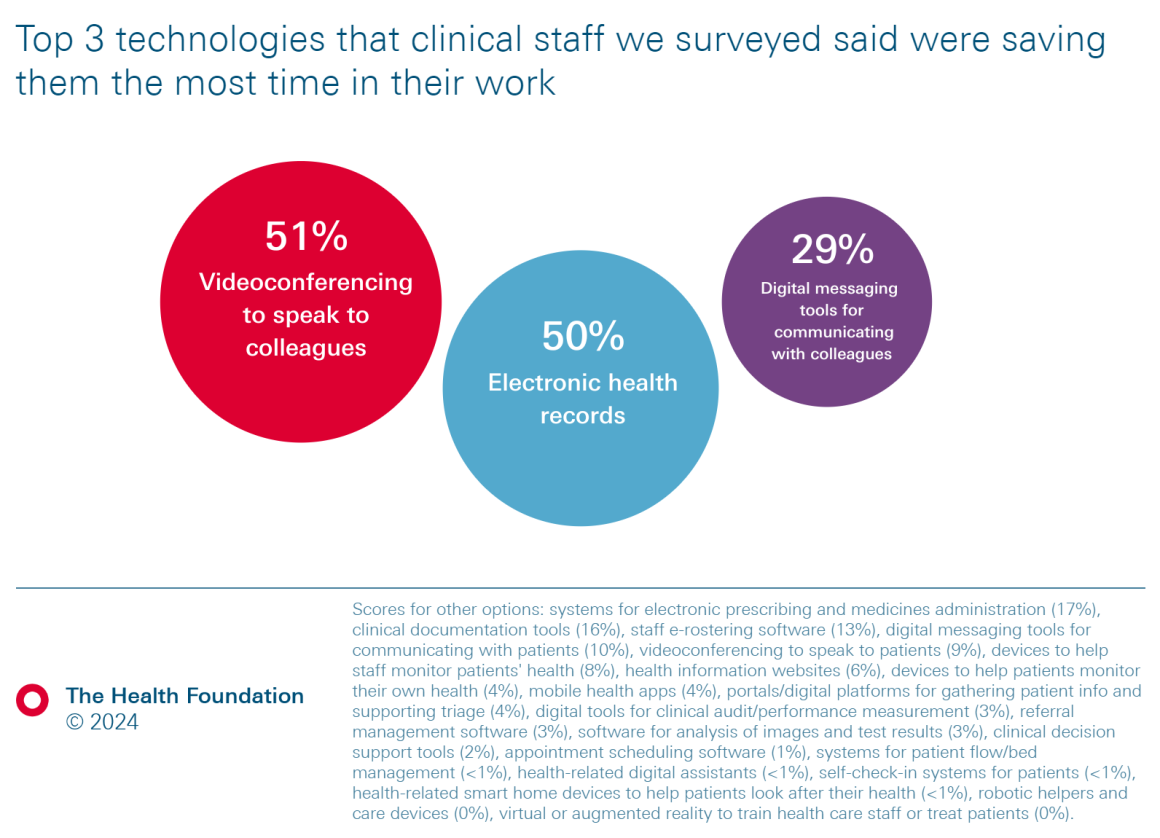
- Our survey found that electronic health records (EHRs) and tools for professional-to-professional communication (including videoconferencing and digital messaging tools) ranked highest in terms of which technologies are saving staff time right now. This contrasts with the typical health policy emphasis on cutting-edge clinical and patient-facing technologies. Maximising opportunities to free up time in the NHS will require focusing on technologies that can help with administrative and operational tasks and inter-professional communication as well as clinical tasks.
- Many immediate gains will come from optimising and spreading existing technologies rather than adopting new technologies. Our research found that not only are EHRs helping to save time now, but staff said they were one of the technologies most likely to offer further gains over the next 5 years and beyond. With the vast majority of trusts now having EHRs, it is important to have a strategy in place to realise their benefits.
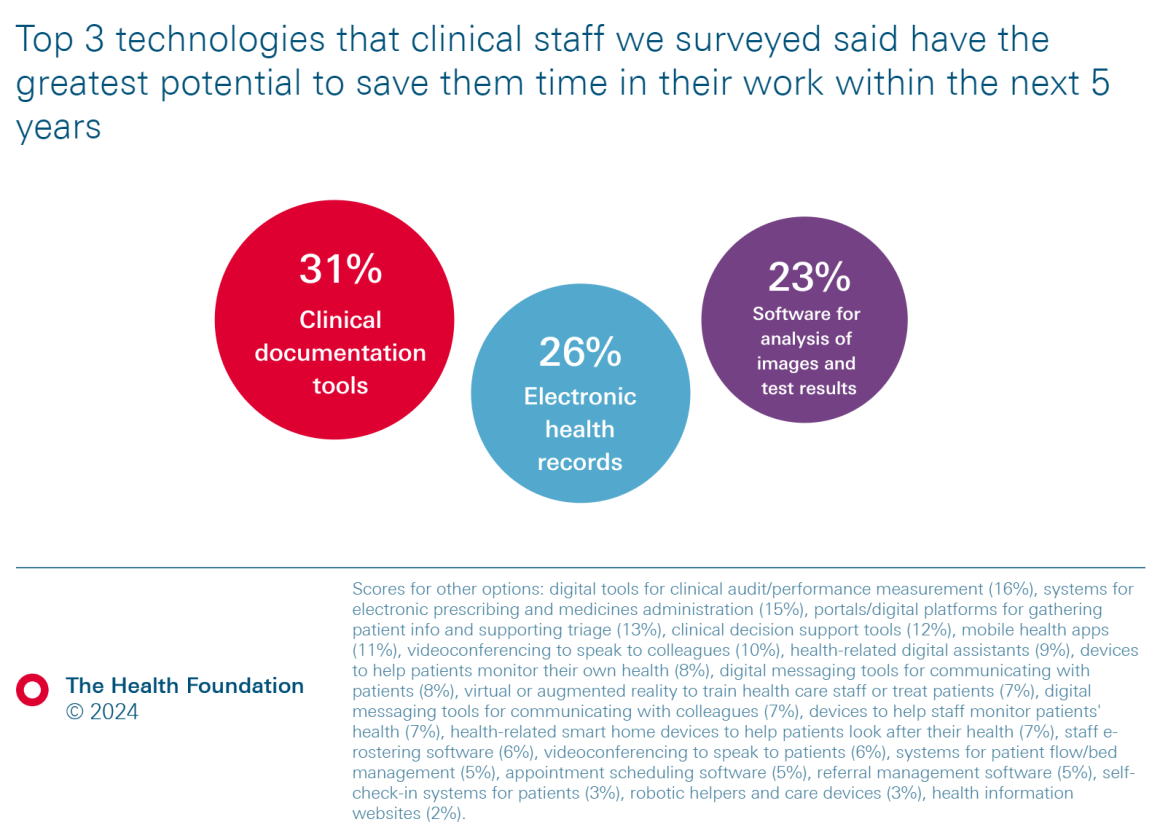
- The clinical staff we surveyed were on balance optimistic about the potential of artificial intelligence (AI) to save them time in their work within the next 5 years. Two of the technologies that ranked highest as likely to save staff time within this period were clinical documentation tools and software for analysis of images and test results – both areas where AI will play a significant role. Our interviewees also highlighted the potential of AI to improve data analysis, risk prediction and population health management. To seize these opportunities, it will be important to look beyond the hype surrounding AI and support rigorous, real-world testing and evaluation of emerging technologies.
- Productivity gains will come not just from technology itself but from how well it is used. We found the biggest barriers staff face in using technologies effectively in their work include underlying IT and digital infrastructure and capability, as well as challenges with implementation and usage. Specifically, we identified considerable frustrations about the lack of IT support, lack of funding to implement new technologies and poor-quality connectivity and equipment. Action is needed to tackle these barriers if the benefits health technologies can offer are to be realised.
- Too often, the development and spread of health technology are driven by suppliers and procurement processes rather than by what the NHS workforce wants and needs. Technology in the NHS is more likely to be successful if staff have greater involvement in demand signalling and the development and deployment of technologies. This will also help build the coalition between policymakers, industry, health care providers and staff that is needed for technology to transform how the NHS provides care.
Our research draws on an anonymous online survey of clinical staff across the UK and semi-structured qualitative interviews with experts on the use of technology and AI in clinical practice.
We targeted eight professional groups in which there are workforce shortages and thus particular hopes for technology to save time and support staff capacity. To reach and represent each group, we worked directly with the relevant professional body:
- anaesthetists (via the Royal College of Anaesthetists)
- GPs (via the Royal College of General Practitioners)
- intensive care doctors (via the Faculty of Intensive Care Medicine)
- nurses (via the Royal College of Nursing)
- obstetricians and gynaecologists (via the Royal College of Obstetricians and Gynaecologists)
- physiotherapists (via the Chartered Society of Physiotherapy)
- psychiatrists (via the Royal College of Psychiatrists)
- radiologists and oncologists (via the Royal College of Radiologists).
The survey and interviews were conducted by the Health Foundation with support from these partners, who collaborated with us on the survey text and interview script.
Partner organisations promoted the survey to their members across their communications channels. It was also shared with practitioners from relevant specialties via the Health Foundation’s own networks. The survey was open between 24 November 2023 and 31 January 2024 across the survey platform Qualtrics. We received 614 completed responses. 54 of these were removed from the final dataset because they did not meet our eligibility criteria, which excluded those not working within one of our specific staff groups, not currently practising (for example, those who had fully retired) or working fewer than 4 hours per week. As the survey asked about current uses of technology and the potential for saving time, we wanted to focus on staff whose practice exceeded a minimum number of hours. These criteria left 560 eligible responses, which we used for our analysis and reporting.
For the qualitative interviews, partner organisations connected us with experts on the use of technology and AI in their respective specialties or staff groups. We conducted 17 video interviews between January and April 2024. The details of our interviewees appear in the acknowledgements.
We also commissioned the Evidence Centre to carry out a rapid review of the evidence base on the impact of digital and telephone technology on staff time in health care to help us understand the scope of literature. The review drew on published and unpublished studies available in English from any country between January 2010 and September 2023. The review was designed to provide an indication of the body of literature on this topic rather than to undertake a systematic review or a critique of the evidence base, and we deliberately set broad parameters. It sampled 500 studies most relevant to our search parameters on the impact of digital and telephone technology on health care staff time and workload.
Indeed, the role of and potential for technologies to support administrative and operational work and inter-professional communication was a prominent theme in interviews as well as the survey. Reflecting on opportunities across both primary care and the wider NHS, Toyosi Adeniji (GP Partner and national First5 Chair, Royal College of General Practitioners) commented that ‘technology has huge potential to release time in routine administrative tasks,’ adding that it ‘really helped [with] communication between some specialties.’
The rankings of videoconferencing to speak to colleagues and digital messaging tools for communicating with colleagues seem especially significant. In the wake of COVID-19, there has been considerable interest in technologies for patient-facing communication (for example, telehealth), but tools to support interaction between staff – even those as relatively simple as Microsoft Teams – have attracted far less attention in policy discourse. This is despite research showing that ‘social technologies’ that can improve communication and collaboration among employees may offer significant productivity benefits for organisations.
The evidence on whether EHRs save time is mixed, as indicated by the rapid evidence review we commissioned (see Box 1). Of 72 studies about EHRs and related tools identified in the review’s sample, 56% found staff time savings, while 44% found no time savings. There were similarly mixed results in the evidence base around some of the more novel clinical technologies, such as robotic-assisted surgery. (Though it should be noted that this was not a systematic review of the evidence and, as such, the findings need to be interpreted with caution.) Our own analysis of the literature suggests that one key reason many reviews of technology find mixed results is differences in the effectiveness of implementation across different contexts.
It is notable that the highest-ranking technologies in our survey – EHRs (and the access to data they permit) and tools for inter-professional communication – are both central to helping the NHS move towards more joined-up, integrated care for patients. However, the interviews and survey responses also indicated significant concerns that EHRs in particular are not yet being used effectively or to their full potential. Several interviewees described in detail the frustrations they encountered in being unable to access notes and test results from other providers, leading to time-consuming efforts to contact colleagues from other sites to track down patient information. This highlights some of the challenges the NHS faces with interoperability and data sharing, where there is clearly substantial scope for improvement.
Our survey and interviews focused on clinical professions; more work is needed to gather insights from non-clinical staff. For example, only one survey respondent selected self-check-in systems for patients as saving the most time in their work. This may not reflect the time-saving potential of this technology for the NHS, but rather that the work of checking in patients tends to sit with administrative rather than clinical staff. Our survey also asked respondents what saved them time individually as opposed to what saved time for their team, department or the wider NHS. These broader issues were explored in the interviews and in our wider stakeholder engagement. Notably, while our expert interviewees did mention more niche clinical technologies that might save time within their particular professional discipline, there tended to be greater interest in general use technologies that would save time across the NHS more widely.
Significantly, our findings suggest there are gains to be made from technologies that are not yet widely used, with only 39% of respondents reporting they have used clinical documentation tools and only 13% reporting they have used software for analysis of images and test results. It is perhaps unsurprising that staff across different groups felt technology that supported these activities could release time, given the burden of clinical documentation across settings and the reliance of so many patient pathways on imaging and test results.
We also asked survey respondents to what extent they thought AI will save them time in their work within the next 5 years. 57% said this is either somewhat or very likely (see Figure 3). This indicates reasonable optimism among clinical staff about the potential time-savings from AI in the near future. Similarly, among our interviewees, while AI technologies were not perceived as making a significant difference to work in the NHS right now – largely because their use was seen as patchy and uneven – there was hope about realising benefits in future. Nevertheless, several interviewees expressed caution about some of the aspirations surrounding new technologies. Nick Woznitza (Consultant Radiographer, University College London Hospitals and clinical academic, Canterbury Christ Church University) warned that ‘AI is not going to save the world in and of itself’. There was scepticism about some of the hype – perhaps unsurprising given challenges to effective implementation of AI within the NHS due to factors such as poor IT infrastructure, problems with data quality and concerns surrounding the potential impact on health equity. Despite the need to address these challenges, interviewees also identified how AI functionalities could be plugged into and optimise existing technologies, like EHRs.
Figure 3
AI will also play a significant role in the other two technologies ranked highest by respondents as likely to save them time within the next 5 years: clinical documentation tools and software for the analysis of images and test results. One example of the former is AI-driven ambient voice technology (AVT), which uses voice-to-text software to auto-transcribe patient consultations and then natural language processing to turn these transcriptions into summary notes and letters. Asif Bachlani (Consultant Psychiatrist, Priory Group and Associate Non-Executive Director, Kent and Medway NHS and Social Care Partnership Trust) indicated that voice recognition technology could offer ‘a massive reduction in the admin burden for front-line clinical staff’. Ben Jeeves (Associate Chief Clinical Information Officer, Clinical Safety Officer and Advanced Practice Physiotherapist, North Integrated Musculoskeletal Service, Midlands Partnership University NHS Foundation Trust) similarly highlighted the ‘heavy burden’ of admin and imagined a future where AVT could lead to ‘the complete removal of the admin processes associated with all of the clinical interactions that we have now to then give us far better quality in terms of the consultations that we’re having, how we interact with our patients’.
When it comes to software for the analysis of images and test results, some of the more ambitious aspirations about their time-saving potential may take a while to realise. Stephen Harden (Consultant Radiologist, University Hospital Southampton and Vice-President for Clinical Radiology, Royal College of Radiologists) told us about his experiences with AI-enabled lung cancer screening, where the current technology effectively identifies possible lung nodules and measures them. ‘It doesn't speed me up a great deal, but it does to some extent’, he noted, but also emphasised that the technology offered ‘real benefit’ in helping to maintain the quality of image interpretation. Longer term, however, there is considerable interest in the potential for AI to act as a ‘pre-reader’ for images, which could offer a more transformational way to save time and support workforce capacity. As Harden explained, ‘the hope is that when reliable and accurate AI is fully developed and implemented, there would be really helpful assistance to radiologists and imaging departments’.
In the rapid evidence review, the sample of 500 studies found a potentially promising evidence base for the time-saving possibilities of automated screening and interpretation of test results, X-rays, patient records, voicemails, and so on. Of the 34 studies in this space included in the sample, 85% reported a positive impact on staff time. As the review noted, however, newer technologies tend to have less evidence available about their impacts, and studies with positive findings may be more likely to be published than those where new technology did not work well. In contrast, more established technologies like EHRs have generated a broader evidence base, which is more likely to contain studies with mixed or negative findings.
Imagining which technologies could release time beyond the immediate future requires a significant degree of speculation. The exploratory nature of the interview format helped us to grapple with the nuances of this question. We asked experts to comment on potential opportunities over the next 10 years and then 20 years and beyond – though many interviewees remarked on the inherent difficulty of envisaging these longer-term time horizons.
Several interviewees discussed the potential of AI and other innovations to improve data analysis to support patient care and wider population health. Experts talked about a more ‘proactive’ model of care, whereby AI could generate intelligence about a patient’s health or identify individuals or groups at risk of developing certain conditions or in vulnerable circumstances with the aim of targeting earlier interventions and supporting patient self-management. Interviewees described how this could not only improve patient health and tackle health inequalities but also potentially reduce demand and create more capacity in the system:
We already have the data in front of us. It's how we use it. And I think if we start to learn how to use that data that is already available, then we could really make a difference and we could actually save a lot of time if we are automating some of that information gathering and those analytics... If you're identifying things early, whether it's disorders, whether it's risks, whatever it is, if you identify it earlier, it will save you time in the long run.
Faith Ndebele, Consultant Psychiatrist, Solent NHS Trust and Chair, Digital Psychiatry Special Interest Group, Royal College of Psychiatrists
That would be enormously powerful, if I could use my voice assistant within an EHR to ask, ‘This patient’s blood pressure’s a bit low, what in the last 24 hours could I have done differently to stop that happening?’ And then [for the technology] to look through all the blood results, medications, etc. and then to come [up] with the relevant information. That would be the most useful thing I could think of. It would save so much time.
Joseph Alderman, Anaesthetic and Intensive Care Registrar, University Hospitals Birmingham NHS Foundation Trust and doctoral researcher, University of Birmingham
Interviewees also acknowledged the barriers to realising these ambitions, however, including variable data quality and the need to develop greater data analytical capability among the NHS workforce.
Figure 4
The prominence of these kinds of reported barriers is perhaps unsurprising, given that successful technology use requires embedding it effectively in local contexts and having the right skills and ways of working to derive the benefits. As noted, it is not uncommon for systematic reviews of the effectiveness of technologies to find mixed results; a central reason for this is that gains from technology are contingent on effective implementation and use rather than simply the technology itself. Further, time savings may be distributed across different staff groups in complex ways that can be hard to measure.
The relevance of context for realising the benefits of technology was also highlighted in our interviews. Dawn Dowding (Professor of Clinical Decision Making, University of Manchester and Co-Chair, Digital Nursing Forum, Royal College of Nursing) told us that while experiences of using a particular piece of technology might be positive in some places, ‘you can have individuals that use the same technology but work in a different organisation and their experiences will be very poor and that's nothing to do with the technology and much more to do with organisation and culture and implementation’.
It is notable that, in our survey, staff and patient concerns about or resistance to technologies were among the lowest-ranked challenges. When presented with a list of barriers, only 12% of respondents selected staff concerns about patient safety and clinical effectiveness, while 10% chose patient resistance to using technologies and 8% chose staff concerns about data protection and security. This does not mean that these issues do not present challenges, however. In particular, some survey respondents (when given free-text fields to expand on their answers) and interviewees referred to encountering resistance among some staff, which they typically framed around scepticism towards technology and/or poor digital literacy. This indicates the ongoing need to both secure staff support for the use of technologies and provide training to improve digital skills and confidence across the workforce. In our survey, 28% of respondents chose ‘lack of time for staff to train’ as a major barrier to using technologies effectively, followed by almost 1 in 5 who said there was ‘not enough training available for staff’. As Adrian Hayter (GP Partner and Medical Director for Clinical Policy, Royal College of General Practitioners) explained, ‘unless we also invest in the training, education and development of people, we're not going to use technology to the best of our ability’.
Some respondents and interviewees complained about the quality of technology procured by the NHS, in some cases even highlighting that their workplace equipment was inferior to the modern technology they used in their personal lives. For example, one survey respondent elaborated in a free-text comment that technology in the health service is done ‘on the cheap’, adding, ‘my set up at home is more advanced than my NHS office set up’.
When it comes to optimising existing technologies (including EHRs), our interviewees suggested that interoperability, user experience and functionality are key areas for improvement. Sandy Jackson (Specialty Trainee in Anaesthetics and Intensive Care Medicine and National Institute for Health and Care Research doctoral fellow at the University of Southampton) told us:
My hope is that some of the biggest opportunities over the next 5 years are improving the user experience and the user interface of existing technologies. So, actually making computer systems that are easier and better for clinicians to use, that work faster and can actually predict some of the things that clinicians might want to input.
Further challenges cited in our interviews included the ongoing need for rigorous testing and evaluation of technologies. Several interviewees also raised concerns about a lack of clinician involvement in technology development and procurement, with the consequence that the solutions being implemented are not always best suited to the needs of the NHS and clinical practice. Dawn Dowding described how, ‘quite often, what you end up with is technology companies coming to you with a solution looking for a problem to solve’, and she identified significant scope for greater engagement with staff. Similarly, Joseph Alderman said it would be positive to move towards a future where technology is seen as ‘something that is developed with clinicians and patients rather than something that is kind of developed for them and then applied to them’.
Further reading
Work with us
We look for talented and passionate individuals as everyone at the Health Foundation has an important role to play.
View current vacanciesThe Q community
Q is an initiative connecting people with improvement expertise across the UK.
Find out more